Hypoxia occurs when the body's tissues don't get enough oxygen. Suffering from this issue can lead to breathing difficulties, an increased heart rate, confusion, and many other problems.
Cells in our body need oxygen to work, and DNA manages all genetic information about how we are built and operate. Therefore, a lack of oxygen can create issues throughout the body, resulting in various harmful impacts.
Symptoms of hypoxia can vary significantly among patients as it relies on which parts of the body are receiving insufficient oxygen, leading to different health problems.
Continue to read the article for a better grasp of what hypoxia means. It poses a risk and is detrimental to your existence. Does this cause persistent issues that complicate matters? How can we resolve it, and is it possible to eliminate it permanently? These and many other questions are going to be answered in the article.
To talk about the effects of low oxygen on our body, it is essential first to understand the process of regular breathing![]() . People with good health inhale oxygen into their lungs, reaching tiny sacs known as alveoli at the ends of small tubes. The oxygen must pass through a person's mouth and travel down their breathing paths first. After this journey, tiny vessels known as capillaries begin their function. These are the smallest ones inside our body, close to the air pockets; they make a pathway for oxygen to move toward human cells. It is crucial to keep in mind that the transport of oxygen occurs solely via blood cells. Therefore, we must maintain an adequate supply of healthy ones.
. People with good health inhale oxygen into their lungs, reaching tiny sacs known as alveoli at the ends of small tubes. The oxygen must pass through a person's mouth and travel down their breathing paths first. After this journey, tiny vessels known as capillaries begin their function. These are the smallest ones inside our body, close to the air pockets; they make a pathway for oxygen to move toward human cells. It is crucial to keep in mind that the transport of oxygen occurs solely via blood cells. Therefore, we must maintain an adequate supply of healthy ones.
Considering this, we discuss how reduced oxygen alters body functions and impacts well-being. This occurs through a modification in the distribution of oxygen within the body. The main reason for the alteration in breathing during hypoxia is that certain body parts do not get sufficient oxygen. Oxygen faces obstructions during travel within the body at particular points.
At times, there isn't sufficient oxygen. This can be a minor issue or turn into a significant danger depending on the cells that are getting too little oxygen to work correctly. Without this, they cannot work properly and might even die. So, the level of danger depends on how much hypoxia there is. If oxygen is not enough for several hours, it can harm vital parts of the body, like the heart or brain, and could cause big health issues or possibly death.
Professionals unanimously identify four types of this condition: anemic hypoxia, hypoxemic hypoxia, histotoxic hypoxia, and circulatory hypoxia. Now, let us embark on a comprehensive exploration of each term; our understanding of these medical terminologies is paramount.
The vastness of the medical dictionary may overwhelm you, yet ‘anemia' and ‘anemic' likely resonate with you. These words might conjure images of weakness, illness, fatigue, or dizziness in your mind's eye. While this information does not come from a medical professional, it stands true to affirm that individuals suffering from anemia indeed have a deficiency in red blood cells. Diminished oxygen transport throughout the body results from a reduced presence of red blood cells in circulation.
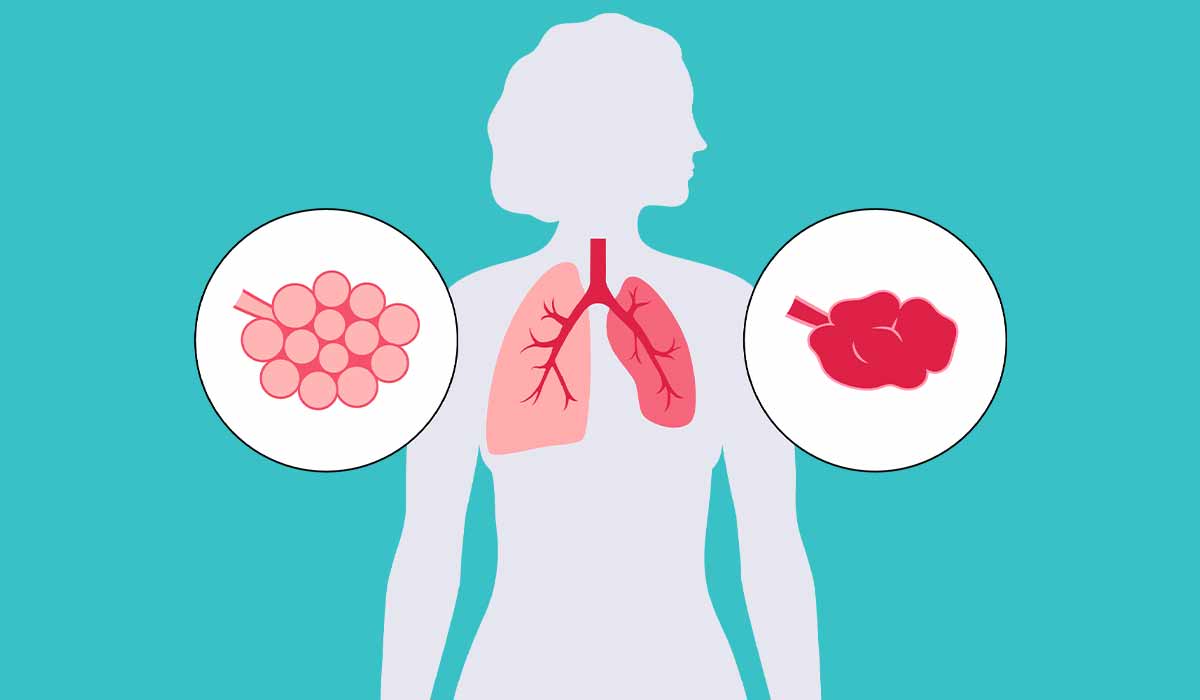
We recall this fact: ‘anemic hypoxia,' a term that resonates with anemia – also referred to as ‘anemic hypoxia' in medical discourse; it results from a primary cause of red blood cell deficiency![]() , subsequently causing reduced oxygen levels.
, subsequently causing reduced oxygen levels.
“Hypoxemic hypoxia,” despite its frequent encounter as a term, presents specific difficulties: it signifies the most commonly found type of condition resulting from inadequate oxygen in the blood. This particularity manifests regularly and originates primarily from standard factors; notably, therefore, is its predictable occurrence. During your visits to high-altitude areas or when certain drugs interact with your body, this may be an experience you encounter. This condition can also result from congenital heart disabilities, lung-related diseases, or issues that compromise the efficiency of cardiac function.
Histotoxic hypoxia occurs when the body's cells do not adequately utilize oxygen. Thus, your belief that you are indeed receiving all of your necessary daily oxygen – even with a plentiful supply within the body – might not be accurate due to various factors impeding adequate intake by these cells; cyanide poisoning is one such reason.
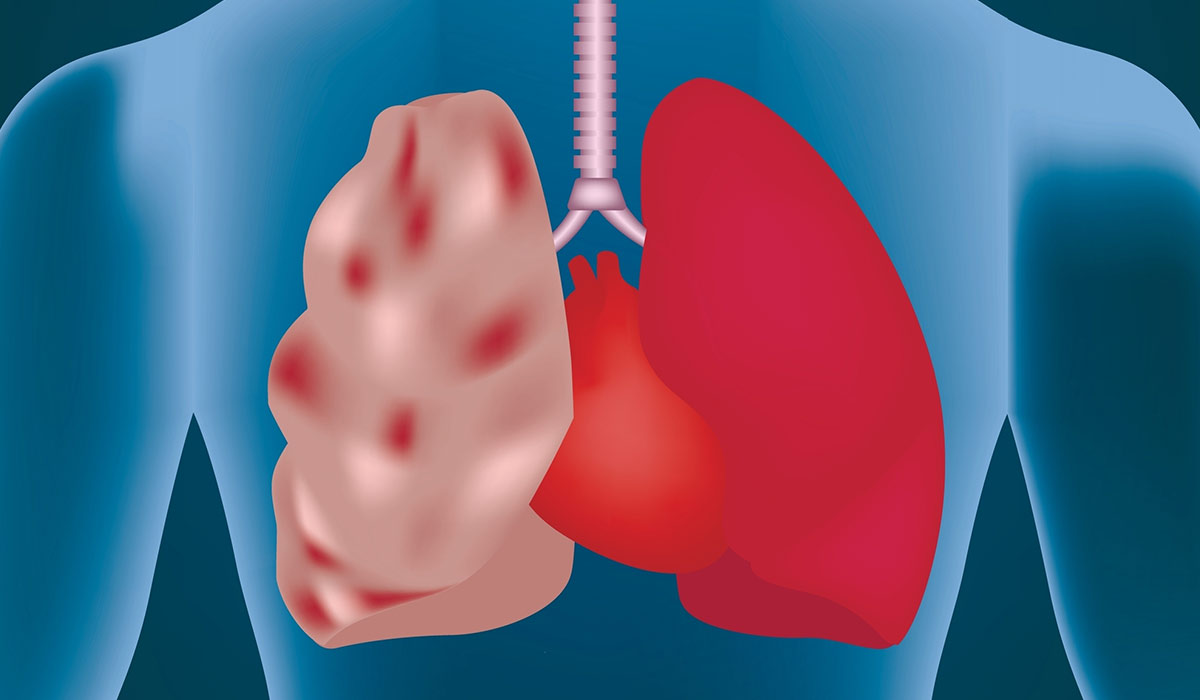
Now, let's delve into the final type: circulatory hypoxia; this condition is intricately tied to heart function. Your physician might refer to it as stagnant hypoxia–or, more alarmingly–potentially ischemic hypoxia.
This scenario mirrors histotoxic hypoxia, where the body indeed abounds with oxygen. However, inadequate cardiac pumping action – a consequence of either heart problems or insufficient blood flow – impedes it from utilizing this plentiful supply. Moreover, sometimes, responsibility for such conditions may also lie with a blockage within a blood vessel.
Often, when a person gets hypoxia, it is because they have other health issues. Typically, there is one particular sickness causing the hypoxia. Below, we listed the most likely conditions that can cause hypoxia:
Similar factors for these conditions are not proper breathing or blood circulation. It makes the supply of oxygen or its usage by the cells not work well. Moreover, some individuals experience low oxygen levels due to injuries that might happen from harm to the lungs.
Hypoxia and hypoxemia![]() are similar-sounding medical terms, which can be problematic. The fact that they are sometimes used interchangeably adds to the confusion. Both hypoxia and hypoxemia involve an insufficient supply of oxygen, but they don't mean the same things.
are similar-sounding medical terms, which can be problematic. The fact that they are sometimes used interchangeably adds to the confusion. Both hypoxia and hypoxemia involve an insufficient supply of oxygen, but they don't mean the same things.
While hypoxia refers to low oxygen levels in cells in tissues, hypoxemia is a term specialists use when there is not enough oxygen in the blood. Hypoxia may stem from hypoxemia, but not in 100% of cases. It is also important to note that a person can have hypoxemia but not suffer from hypoxemia.
Because many tissues and organs can be affected, symptoms between people can vary. Here are the issues observed the most often:
Sometimes, hypoxia can take a severe form and cause a severe inability to relax (restlessness), more serious problems with breathing, and cyanosis (skin turning to blue). When severe problems arise, don't hesitate to call an emergency immediately.
Hypoxia may affect you no matter how old you are. However, older age and other factors increase the risk of developing this condition. Here are the most common ones:
Medical professionals employ various methods to assess their patients for hypoxia: chest X-rays, magnetic resonance imaging (MRI), computerized tomography (CT scan); pulse oximetry and pulmonary function tests (PFTs). Each option undertakes a comprehensive approach–a fact revealed upon closer examination.
The chest X-ray: it provides images of the lungs, assists in identifying alterations or abnormalities associated with lung health. Furthermore—this diagnostic tool is instrumental; it helps determine whether a patient grapples with lung diseases or pneumonia – conditions that potentially trigger hypoxia.
Specialists utilize Magnetic Resonance Imaging (MRI) to discern the presence of hypoxia within an individual, as it produces intricate images of the chest, brain, and various body parts.
The CT scan serves a purpose similar to an MRI; however, it may warrant recommendation in specific cases despite generally providing less detailed results than an MRI.
The pulse oximetry test![]() : a healthcare professional undertakes it by affixing a sensor to the patient's finger or earlobe, gauging their blood oxygen levels.
: a healthcare professional undertakes it by affixing a sensor to the patient's finger or earlobe, gauging their blood oxygen levels.
The Pulmonary Function Test (PFT) assesses the optimal functioning of your lungs, specifically during inhalation and exhalation.
Evaluating the acid, oxygen, and carbon dioxide levels in a patient's bloodstream is what the arterial blood gas (ABG) – a mere blood test – does; an abundance of acid could signify lung and kidney function complications.
An echocardiogram (ECG) – a test that uses ultrasound waves to produce heart images – measures cardiac performance and identifies any notable variations or abnormalities. Since heart disease can trigger hypoxia, choosing an ECG could provide benefits by assisting in the assessment of potential outcomes related to these conditions.
EKG: Electrocardiogram (EKG) assesses the heart's rhythm and rate by checking its electrical activity.
To diagnose hypoxia, your doctor may need to conduct one or more tests: the complexity of your case, the severity of symptoms you exhibit – and any coexisting conditions – will influence this necessity. Thus, heeding your physician's advice becomes imperative: complying with all recommended examinations is crucial—not overlooking their significance—in formulating a precise diagnosis.
Numerous medical conditions may cause hypoxia, necessitating a personalized treatment approach for each individual affected. The overarching objective of this customized therapy remains constant: to furnish tissue with an ideal oxygen supply and prevent severe damage.
Here are the available treatment options that address hypoxia:
Supplemental oxygen therapy represents one approach for ameliorating cases characterized by an inadequate supply of oxygen in the tissues; this condition is known as chronic hypoxia – a state wherein pure breaths of additional oxygen are offered to combat persistent tissue-level deprivation, thus introducing graduate level punctuation.
In some cases, hypoxia may cause dangerous symptoms that need to be addressed as quickly as possible. These include confusion, increased heart rate, and blushed skin, lips, or nails. Treating severe hypoxia early increases the outlook and reduces the risk of complications. If you are not sure if your symptoms indicate hypoxia or other severe conditions, visit your healthcare provider to receive a professional assessment of your health.
Hypoxia is a risky state, yet it's possible to reduce the likelihood of its occurrence. Addressing or controlling these conditions is crucial since other health issues can lead to its onset. However, it might be difficult to prevent it if there is a serious or long-term condition underneath.
However, it is important to look after your health and obey certain safety rules. For example, when you do things where the oxygen might be limited, using trustworthy equipment made by experts becomes essential. These activities, like going to places with high elevations or underwater diving, can be risky for your well-being if you are not adequately ready. If that happens, you might require assistance from a doctor.
Stopping smoking and avoiding tobacco products is good for health and lowers the chance of lung problems, such as hypoxia. If you need nicotine, try to use less or stop using it completely for better health outcomes.
Bettering sleep hygiene and quality might help prevent hypoxia. Sleep disorders like sleep apnea![]() that occur during sleeping times can cause oxygen levels to become unstable when asleep, which can cause hypoxia. Therefore, ensuring sound sleep quality is vital to avoid these issues.
that occur during sleeping times can cause oxygen levels to become unstable when asleep, which can cause hypoxia. Therefore, ensuring sound sleep quality is vital to avoid these issues.
Another significant element is to drink enough water. If you do not consume sufficient water (dehydration), it can change the thickness of your blood and lower the movement of oxygen. So ensure to stay adequately hydrated to maintain optimal blood flow.
Being around chemicals and poisonous gases might lead to a lack of oxygen. This could occur at work or while engaged in specific tasks. To protect yourself against harmful chemicals and toxins, make sure to take the right safety measures and wear protective gear when needed.
Hypoxia is when the body's tissues do not get enough oxygen, which causes different health problems. Cells require oxygen to work correctly; without it, the whole body can be affected and might experience serious damage. The severity of hypoxia depends on factors like duration and affected body parts.
Many health problems can cause hypoxia, such as heart failure, diseases of the lungs, having low blood count (anemia), asthma and others. When breathing or blood circulation is not right, it affects how much oxygen gets through, and injuries can also hurt the lungs, causing hypoxia.
Symptoms can differ but often involve fast breathing, a quicker heartbeat, feeling confused, perspiring more than usual, and changes in the skin's color. In very bad situations, there might be agitation, significant difficulties with breathing, and the skin turning blueish.
Doctors and nurses perform different types of examinations like imaging the chest with X-rays, using MRI machines, CT scanning technology, measuring oxygen in blood by a device clipped to a finger, and taking blood samples for analysis to find out if there is hypoxia and what's causing it.
The goal of treatment is to bring back the best possible oxygen level for the body. This can involve medicine, extra oxygen, using machines that help with breathing, or sometimes, when it's really serious, a ventilator to breathe for you.
Though it's not always achievable to stop hypoxia, living healthily, taking care of any health issues, and being careful in certain places can lower the danger and help with general health. It is important to have frequent medical examinations to find problems early and deal with them.
Table of Contents

Chronic obstructive pulmonary disease, a condition commonly known as COPD, is the third most frequent cause of death in the… read more »

A pulmonary embolism develops when a clump, most often a blood clot, gets stuck inside the lung blood vessel. It… read more »

Lung Cancer begins in cells lining breathing entries, regularly starting with bronchial tubes or minor discuss sacs. It may be… read more »
A pulmonologist is a medical doctor who specializes in diagnosing and treating diseases of the respiratory system, which includes the… read more »
Atelectasis is a lung condition in which parts of the alveoli, tiny air sacks in the lung, lose air. When… read more »

Altitude Sickness is a condition often faced by eager mountain climbers. Dive into our article for more details on this… read more »
Hypercapnia is a condition in which the partial pressure of carbon dioxide in our blood is increased. This can be… read more »
Emphysema is a lung disease that involves excessive aeration of the lungs, which disrupts gas exchange in the body. How… read more »

Dyspnea, which individuals also call shortness of breath, occurs when somebody feels awkward while breathing or suddenly realizes they have… read more »