Hypercapnia is blood's increased carbon dioxide partial pressure. It signals a high concentration of carbon dioxide in our air or body during metabolism. In humans, elevated levels can lead to unsmooth breathing or lung circulation.
Its causes are typically linked to respiratory system diseases. These warning signs need attention from a doctor if they continue for a long duration. If you have serious hypercapnia symptoms, your body is struggling to balance oxygen and carbon dioxide levels.
It is essential to treat the cause of both respiratory failure and hypercapnia. The diagnosis of hypercapnia is based on a test to determine the level of carbon dioxide in the blood. Oxygen therapy often improves the patient's condition and normalizes gas parameters. If a patient with hypercapnia does not receive appropriate treatment, severe complications may result. This is particularly true of chronic hypercapnia, which can be fatal.

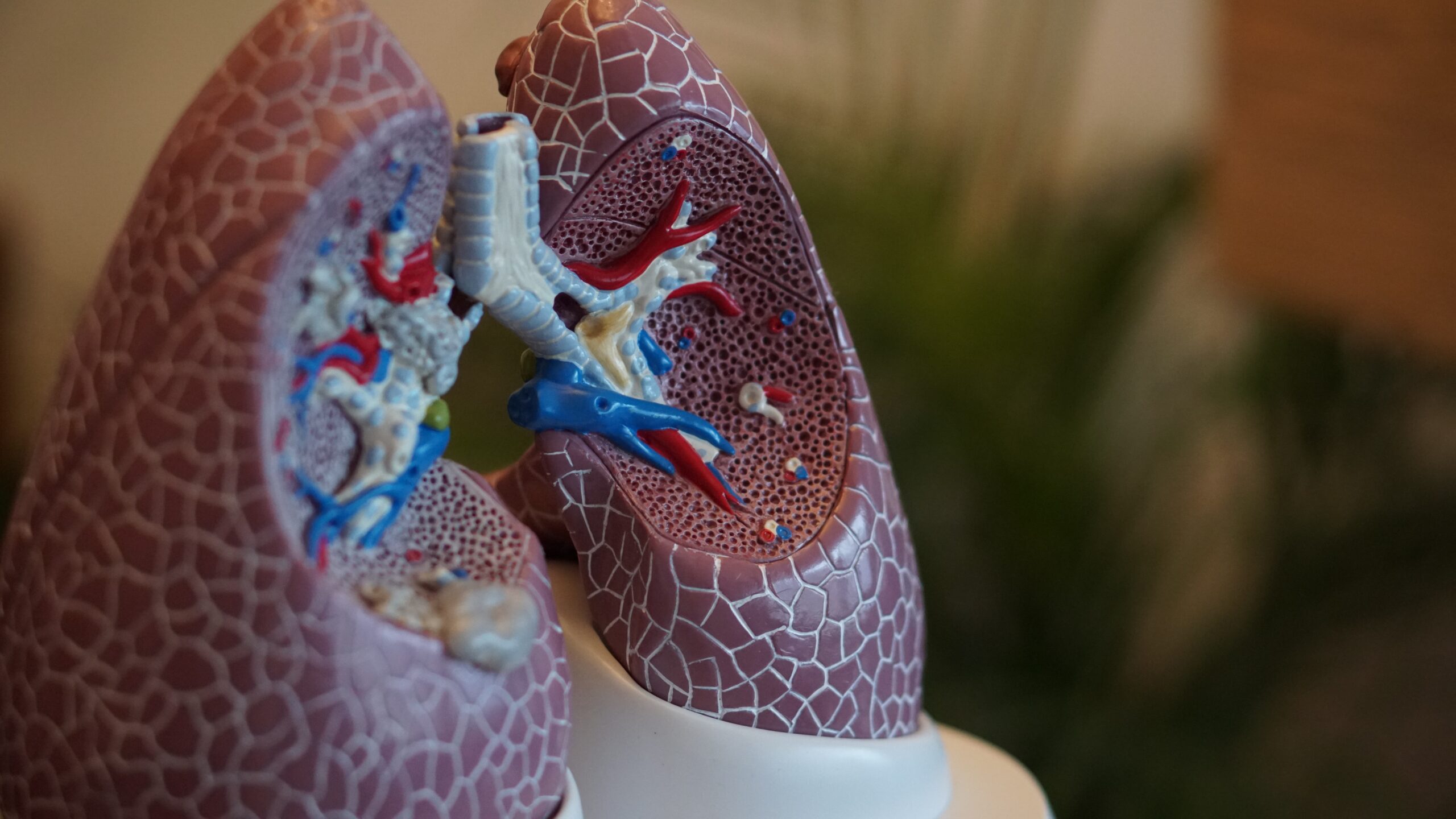
The mechanisms leading to hypercapnia are many and varied. The scientific literature describes risk factors associated with developing chronic hypercapnia in patients. People with impaired lung ventilation![]() are primarily at risk of hypercapnia. But other factors can also increase the risk of hypercapnia. These include:
are primarily at risk of hypercapnia. But other factors can also increase the risk of hypercapnia. These include:
Respiratory problems – This is the leading risk factor for hypocapnia. Respiratory problems can have many causes. Weakened inspiratory muscles may contribute. Airway obstruction that makes breathing difficult can also contribute to hypocapnia. Bronchospasm or swelling of the mucous membrane obstructs the lower airways. An increase in the amount of air lingering in the airways not involved in gas exchange is also dangerous. People with conditions such as asthma, obstructive lung disease, and obstructive sleep apnoea are at risk of hypocapnia.
Smoking – This habit has many adverse health effects, including a higher risk of hypocapnia. It is well known that smoking cigarettes is bad for the respiratory system. Tobacco smoke irritates and damages the laryngeal mucosa, leading to symptoms of chronic laryngitis as well as laryngeal cancer. Smoke also harms the rest of the respiratory tract, causing swelling and airflow obstruction. With the onset of hypercapnia symptoms, the absolute prohibition of smoking is most important.
Obesity – This condition is recognized as a disease that also causes numerous health complications. These include hypercapnia. The respiratory system is significantly affected by obesity. In addition to exertional dyspnoea and reduced physical capacity, it can harm respiratory mechanics, especially in people with respiratory disease. Increased incidence and severity of respiratory infections may be associated with obesity. Therefore, a change in diet may also be necessary in people with hypercapnia.

The primary process leading to hypercapnia is alveolar hypoventilation![]() . Alveolar hypoventilation refers to two processes leading to reduced respiratory drive: reduced central nervous system control and impaired respiratory muscle strength. They increased dead space area due to airways, parenchyma, and vasculature changes.
. Alveolar hypoventilation refers to two processes leading to reduced respiratory drive: reduced central nervous system control and impaired respiratory muscle strength. They increased dead space area due to airways, parenchyma, and vasculature changes.
Hypercapnia occurs when the patient cannot maintain satisfactory ventilation due to respiratory overload. Overload challenges the thoracopulmonary system and results from increased airway resistance and ventilation demand. Pulmonary hyperinflation![]() also plays a significant role. The term is broadly defined as the lung capacity at rest. Despite the presence of compensatory mechanisms, pulmonary hyperinflation impairs ventilation capacity.
also plays a significant role. The term is broadly defined as the lung capacity at rest. Despite the presence of compensatory mechanisms, pulmonary hyperinflation impairs ventilation capacity.
Hypercapnia is most often caused by a specific disease that negatively affects the breathing mechanism. Hypercapnia can also occur due to being in rooms where carbon dioxide concentrations are elevated. Thus, the causes of hypercapnia may include:
Asthma – Asthma is a persistent illness affecting the airways of our body. The bronchi and air tubes suffer enduring inflammation. Its effects vary. Serious situations may create sudden, intense breathing difficulty. The primary trigger is allergy, an extreme body response to usual things in our surroundings. For most patients, the disease is well controlled over a long period. Nevertheless, symptoms may reappear, either suddenly or slowly increasing and posing a risk of hypercapnia.
Chronic obstructive pulmonary disease – This chronic respiratory disorder results in restricted airflow to the lungs. It is characterized by progressive impairment of pulmonary ventilation, chronic airway inflammation, and permanent lung damage. The causes of the disease are varied and include smoking, air pollution in the living or working environment, and respiratory infections in early childhood. Chronic obstructive pulmonary disease poses a high risk because it can be asymptomatic for many years.
Acute respiratory distress – ARDS is when the lungs are seriously hurt. Because of this, they can't supply enough oxygen to the blood. This could lead to other organs failing. Different things can cause ARDS. A virus that brings pneumonia, a physical injury, or serious sepsis are some examples. There are two kinds of respiratory failure—one type happens when you have hypercapnia during the disease progress. If hypercapnia is really severe, it means the person is going through respiratory failure.
Sleep apnoea syndrome – Obstructive sleep apnoea is when physiological breathing stops or becomes shallow during sleep. The condition is referred to when, with increased work of the respiratory muscles, airflow through the upper airway is restricted, often accompanied by snoring. There can be many causes for the onset of sleep apnoea. This condition can occur due to anatomical defects in the respiratory system.
Carbon dioxide poisoning – Various places see a rise in carbon dioxide levels. This could affect workers in polluted environments more. Be chary in spots like dry ice storehouses, garages, or mines. Blocked chimneys or vents can cause carbon dioxide poisoning. Breathing this gas in a confined space can make you unconscious swiftly, leading to death within minutes.
Neurological disorders – Rarer causes include neurological disorders. It includes amyotrophic lateral sclerosis and spinal cord injury. Many progressive neuromuscular diseases can lead to increasing weakness of the respiratory muscles. This, in turn, can lead to nocturnal hypoventilation and gradual progression to respiratory failure. Patients in the advanced stage of the disease have paresis of all four limbs, speech and swallowing disorders, and respiratory failure due to respiratory muscle weakness.
Medications – A common cause of hypercapnia resulting from respiratory muscle impairment is the effect of opioids![]() on the brain center responsible for breathing. Drugs can also lead to this condition. Severe respiratory problems, even leading to death, can occur in patients using gabapentinoids and opioid drugs concomitantly. These drugs are approved to treat a range of ailments. Seniors are particularly at risk.
on the brain center responsible for breathing. Drugs can also lead to this condition. Severe respiratory problems, even leading to death, can occur in patients using gabapentinoids and opioid drugs concomitantly. These drugs are approved to treat a range of ailments. Seniors are particularly at risk.
Muscular dystrophies – Hypercapnia, an ailment, can be caused by issues in your muscles. If you have muscular dystrophy, a common inherited sickness, you might experience drastic muscle weakness. This can lead to your muscles shrinking over time. Difficulty breathing is a usual downside of this genetic disease because your muscles aren't as strong. One good solution is respiratory exercises – they're crucial to physical therapy. These exercises help you get better at breathing and keep your breathing muscle power up for a longer duration.
The average amount of oxygen and carbon dioxide in the blood is influenced by lung ventilation and blood flow through the lungs. The norm for the partial pressure of carbon dioxide in arterial blood is between 32-45 mm Hg![]() .
.
Above these values, hypercapnia is noted. Hypercapnia causes dysfunction of the alveolar epithelium, resulting in alveolar edema and further impairment of gas exchange. Repair mechanisms of the airway epithelial cells are also impaired as the condition causes mitochondrial dysfunction and impaired cell proliferation.
Our body informs us of the state of hypercapnia through symptoms occurring in the nervous and respiratory systems. The body can detect and partially compensate for low oxygen pressure or too high a quantity of carbon dioxide in the blood.
Mild symptoms of hypercapnia indicate the activation of compensatory mechanisms. Severe symptoms of hypercapnia suggest that the body cannot compensate for the amount of oxygen and carbon dioxide. These symptoms are an alarm signal. If they persist over a long period, a doctor should be consulted. Symptoms of hypercapnia include:

Headaches and dizziness – At the start of hypercapnia, you might get a little headachy or dizzy. You can also feel lost, and it might get hard to focus. Hypercapnia means less blood goes to your brain. That means less oxygen for your tissues. This can make your head hurt.
Shortness of breath – In the initial phase of the illness, shortness of breath is present, but the rapid breathing characteristic of a severe hypercapnic state is absent. The person may experience difficulty breathing, a feeling of breathlessness, or shortness of breath.
Skin redness – Lack of oxygen can change your skin, inside your mouth, and fingernails' colors. When there's too much carbon dioxide, or hypercapnia, your skin turns red. Your eyes might also get bloodshot. That's because hypercapnia expands your blood vessels.
Excessive sleepiness or agitation – People with hypercapnia often feel too sleepy and tired, more than they should for their work. If the carbon dioxide level doesn't drop, they feel worn out and wasted. When hypercapnia gets severe, they might feel too stirred up or confused. It can cause panic attacks, or they might feel strangely suspicious or sad. Everyone with hypercapnia has different experiences. Some might feel more restless, others just more tired.
Irregular heartbeat – Heart rhythm issues, or cardiac arrhythmia, involve the heart beating too quickly, slowly, or unevenly. Temporary situations like hypoxia, often caused by hypercapnia, frequently lead to these rhythm problems.
Muscle tremor – In serious cases of hypercapnia, too much breathing can lead to muscle twitching and shaking. Muscle shakes are unintentional, unprompted, repeated muscle moves. This can take place anywhere on the body and range in severity. Body shakes signal poor oxygen supply to the body.
Hyperventilation – People grappling with hyperventilation sense they lack sufficient air. This state may express itself through discomfort, unsteadiness, or extreme tiredness. Continuous hyperventilation symptoms are a tight feeling, problems with vision, headaches, and body shivers. During hypercapnia, an individual might take quick, shallow breaths to balance the boosted carbon dioxide levels in their blood.
Syncope – High levels of carbon dioxide, or hypercapnia, can cause fainting and even loss of consciousness in extreme cases. Too much carbon dioxide might even stop a person’s breathing, especially if they’re getting too much oxygen therapy. This can cause a hypercapnic coma![]() , a serious condition.
, a serious condition.

Hypercapnia means too much carbon dioxide in the blood. It usually shows up with breathing trouble. So, finding out if you have it is important. The best way to check for hypercapnia is by doing a blood gas test![]() .
.
Blood gas test – This involves assessing the blood saturation with carbon dioxide. This allows you to calculate how much of the blood gas is carbon dioxide and how much is oxygen. This enables the severity of the patient's condition to be assessed. The test is simple and quick, simply taking arterial blood from the patient. Gasometry is used to diagnose gas exchange disorders, i.e., respiratory insufficiency, monitor their treatment, and diagnose and monitor acid-base disorders.
If the ventilatory disturbance is caused by aspiration of a foreign body, bronchoscopy may be necessary.
Bronchoscopy – It's a type of examination where doctors can take a close, personal look at someone's lungs and breathing structures. Why would someone need this? Lots of reasons! One could be that doctors suspect a lung tumor. Or maybe someone accidentally breathed in something they shouldn't have. When conducting a Bronchoscopy, doctors use a flexible tube that goes into the patient's body. Fun fact: this is the most popular method doctors use to visualize a person's airways.
In hypercapnia, it is essential to treat the cause. Depending on the severity of hypercapnia, different treatment methods are used. These include:

Oxygen therapy – They often use oxygen therapy![]() to help patients. It makes the gas parameters normal. A mask gives oxygen to the patient. The treatment method is to increase the oxygen in the air the patient breathes. Be careful with very sick patients. Too much oxygen might slow or stop their breathing. That could make the problem with their breathing worse.
to help patients. It makes the gas parameters normal. A mask gives oxygen to the patient. The treatment method is to increase the oxygen in the air the patient breathes. Be careful with very sick patients. Too much oxygen might slow or stop their breathing. That could make the problem with their breathing worse.
Mechanical ventilation – Severe respiratory failure indicates intubation and mechanical ventilation. Mechanical ventilation can be invasive or non-invasive. It is the process of treating respiratory failure by forcing air through the airways. Home mechanical ventilation is the treatment of respiratory failure using a ventilator in a home environment. Mechanical ventilation supports or replaces breathing in patients who do not take their own breaths or whose breathing needs to be supported.
Pharmacotherapy – The use of drugs for treatment depends on the cause of hypercapnia. In the case of pneumonia, treatment will be appropriate antibiotic therapy![]() . In the treatment of asthma, bronchodilators and drugs to reduce bronchial mucosal edema are used. These are mainly beta-mimetics and glucocorticosteroids. In severe cases, medication to combat acidosis may be taken.
. In the treatment of asthma, bronchodilators and drugs to reduce bronchial mucosal edema are used. These are mainly beta-mimetics and glucocorticosteroids. In severe cases, medication to combat acidosis may be taken.
Lifestyle changes – To avoid exacerbations, the main things to do are to stop smoking, take medication regularly, and follow your doctor's instructions. If you are obese, you may need to change your diet and introduce safe exercise and breathing exercises. In situations where hypercapnia is the result of sleep apnoea syndrome, there are specialist clinics where medics treat sleep disorders.
Untreated hypercapnia can lead to dangerous complications. The complications of hypercapnia are usually very severe and involve irreversible changes to specific body structures. Therefore, this condition should be considered and recognized. However, if the patient's condition is well diagnosed and the doctor implements appropriate treatment, the prognosis is generally reasonable. Complications of hypercapnia include:
Respiratory acidosis – Results from excessive accumulation of carbon dioxide in the body due to impaired lung ventilation. When this occurs, the acid-base balance![]() is disturbed. The result is the accumulation of too much gas in the body. The symptoms of respiratory acidosis are non-specific and depend on the nature of its course. If it is acute, severe anxiety, shortness of breath, increased heart rate and respiration, hallucinations, and unconsciousness can be observed. Such a condition requires immediate medical intervention.
is disturbed. The result is the accumulation of too much gas in the body. The symptoms of respiratory acidosis are non-specific and depend on the nature of its course. If it is acute, severe anxiety, shortness of breath, increased heart rate and respiration, hallucinations, and unconsciousness can be observed. Such a condition requires immediate medical intervention.
Cerebral vasodilatation – The consequence of acute carbon dioxide poisoning may be irreversible damage to the central nervous system. Hypercapnia causes cerebral vasodilation and increases blood flow and total blood volume in the cerebral vessels. Hypocapnia causes vasoconstriction and, secondarily, may exacerbate cerebral ischemia. The result of cerebral hypoxia is often paralysis of the limbs and impaired speech or motor coordination. When the brain becomes starved of oxygen, certain nerve cells start to die.
Coronary insufficiency – Carbon dioxide poisoning can lead to coronary insufficiency. Coronary artery disease involves insufficient oxygen and blood supply to the heart muscle. It results from the narrowing of the coronary arteries, which is closely related to atherosclerosis of the blood vessels. The result of coronary artery disease is a decrease in the amount of blood and, with it, oxygen and nutrients delivered to the heart muscle cells.
Myocardial infarction – Lack of oxygen to the heart triggers a heart attack. If blood doesn't flow back fast enough, a heart attack could permanently harm the heart, and sadly, cause death. A sudden, severe chest pain typically indicates a heart attack.
Hypercapnia is when too much carbon dioxide is in the blood. It happens when there's too much carbon dioxide in the air or inside us when we break food down into energy. This can make breathing or blood flow in the lungs less effective. Hypercapnia often starts from not breathing well enough in our lungs. Studies tell us that people with lousy lung ventilation usually have this issue. Some illnesses that affect our lungs cause hypercapnia.
On top of that, staying in rooms high in carbon dioxide can also bring it on. Mild signs of hypercapnia show that our bodies are trying to balance out the oxygen and carbon dioxide. Serious signs show that our bodies can't keep up with this balancing act. To check for hypercapnia, doctors use a blood gas test. It's key to treat the root of hypercapnia. Different ways are used to treat it, based on its seriousness. If ignored, hypercapnia can cause serious problems. So, we need to take this condition seriously.
Table of Contents

Activated charcoal is a substance used for various ailments. The most common use is to treat poisoning. However, charcoal also… read more »

A medical condition known as acidosis is the result of an overabundance of acid within the body's inner liquids, which… read more »

Flatulence is the excessive accumulation and release of gases. See what are the causes of this condition. What to do… read more »
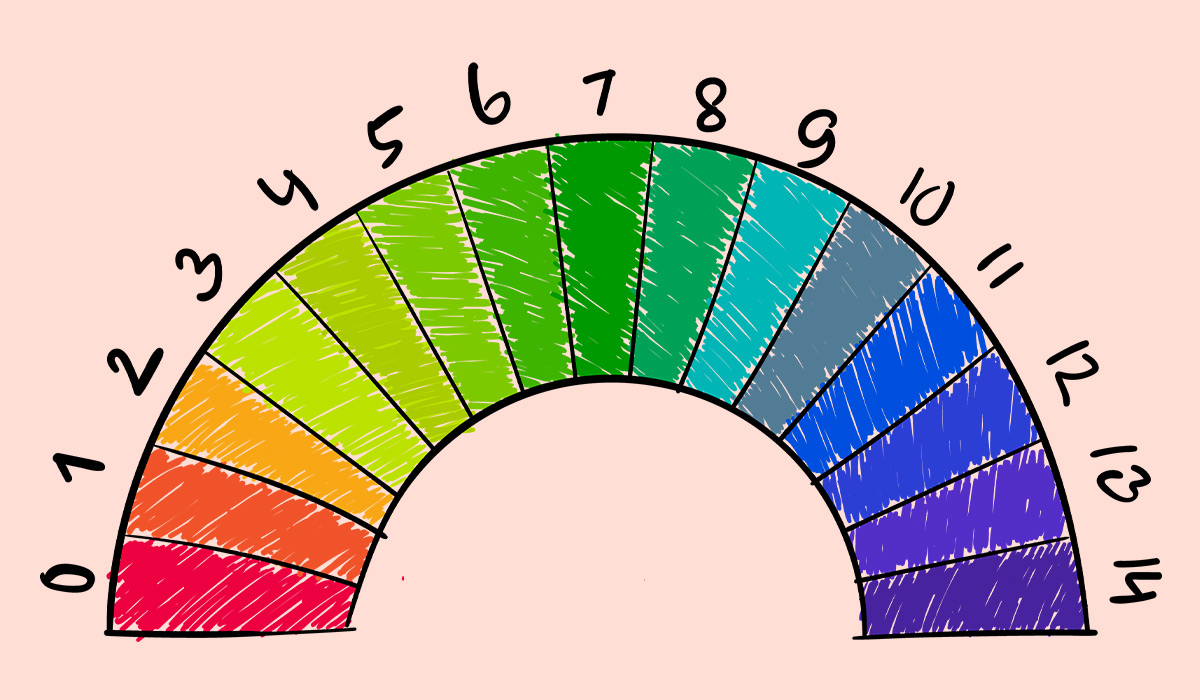
PH balance refers to the level of acidity or alkalinity in a substance, which is measured on a scale from… read more »

Hypoxia occurs when the body's tissues don't get enough oxygen. Suffering from this issue can lead to breathing difficulties, an… read more »

Black mold is a type of fungus that thrives in damp and humid environments. Is it dangerous for health? read more »
Hemoglobin is an important part of the blood. Its deficiency as well as excess negatively affects health. Learn about the… read more »

Dehydration can cause many negative health effects. It is a common problem in children and seniors. Learn how to recognize… read more »

A bloated stomach is a condition characterized by a feeling of fullness, tightness, or swelling in the abdomen. What are… read more »