Altitude sickness refers to the health issues often encountered by passionate mountaineers and climbers. This condition, a common challenge among enthusiasts, entails specific symptoms and requires appropriate remedies. Understanding the symptoms and taking necessary precautions is crucial when dealing with altitude sickness as it is closely associated with specific environmental conditions.
Altitude sickness: Illness is associated with being in specific conditions. This term describes various adverse health effects when living at high altitudes. When people living in the lowlands quickly climb to over 2000/2500 m above sea level, symptoms can occur due to low air pressure and lack of oxygen. Altitude sickness can lead to organ failure, which is an immediate threat to health and life. Its first symptoms should, therefore, not be underestimated. Knowing how to deal with altitude sickness to increase your safety during a mountain expedition is worth knowing.

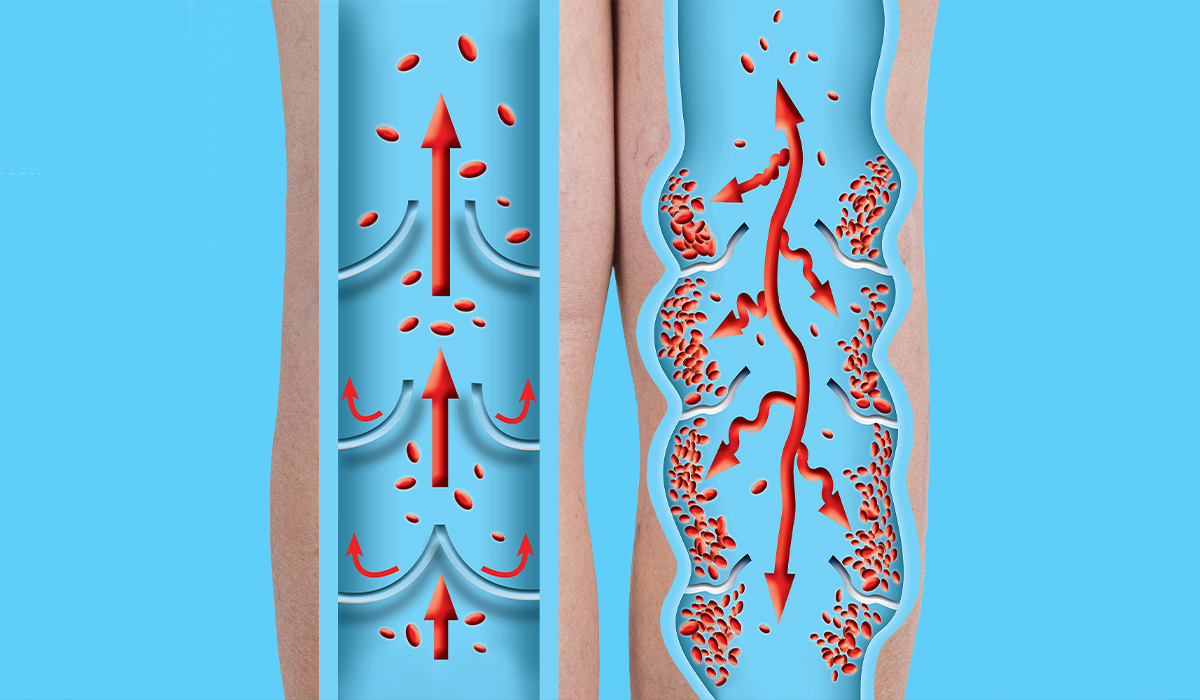
Usually, altitude sickness occurs when the body has not been given enough time to acclimatize, i.e., get used to the difference in altitude. Altitude sickness occurs due to lower oxygen levels in the air and insufficient oxygen saturation in the alveoli, leading to a decrease in blood vessel integrity and subsequent fluid accumulation in the surrounding tissue.
The primary cause of this condition is hypoxia![]() , which is primarily a result of reduced air pressure at higher altitudes. In other words, altitude sickness is a set of conditions that arise from the reduced pressure and oxygen content in the atmosphere. Breathing at altitude provides much less of it than in different areas. Thus, the condition causes specific symptoms and can lead to death.
, which is primarily a result of reduced air pressure at higher altitudes. In other words, altitude sickness is a set of conditions that arise from the reduced pressure and oxygen content in the atmosphere. Breathing at altitude provides much less of it than in different areas. Thus, the condition causes specific symptoms and can lead to death.
Altitude sickness usually appears above 2,500 meters above sea level![]() , but in some special susceptible people, it can appear as low as 1,500 meters above sea level. Traveling to high-altitude areas, such as mountainous regions and certain cities or towns at elevated geographical points, can pose risks. Some well-known high-altitude cities include:
, but in some special susceptible people, it can appear as low as 1,500 meters above sea level. Traveling to high-altitude areas, such as mountainous regions and certain cities or towns at elevated geographical points, can pose risks. Some well-known high-altitude cities include:
Primarily, tourists and travelers are at risk of altitude sickness in these areas. It is crucial to be prepared and prioritize safety when visiting high altitudes. The human body acclimatizes to the thin air gradually during a gradual ascent to higher altitudes. However, ascending too quickly can hinder this process, leading to symptoms of altitude sickness. Additionally, it's important to note that good physical condition does not decrease the risk of illness at high altitudes.

The severity of symptoms depends on several significant factors. These include age, weight, blood pressure values, and respiratory capacity. The rate and duration of ascent to a given altitude are also considered. Symptoms can develop within days of the onset of being at high altitude. Each traveler should know how to recognize the symptoms and how to proceed in the event of illness. To better assimilate the knowledge, we have divided the symptoms into the following syndromes:
Symptoms can occur at 1,500 – 3,500 meters above sea level. Above 3,500 m above sea level, there is a high risk of symptoms. Traveling too fast at altitude can cause mild symptoms. Typical symptoms of Acute Altitude Sickness belong to:
Headaches and dizziness – The main symptom is headache, but it is a vague symptom to recognize the onset of the disease. The symptoms may be subtle, and the sufferer may not notice them. Even if you take painkillers, a bad headache might persist. This could interfere with clear thinking. Feeling dizzy means you sense that you're swaying or spinning, or that you're unsteady or shaky.
Fatigue – You may endure more fatigue and feel achy muscles. A decrease in air's oxygen levels and falling blood pressure can cause fitness and energy to drop, even if you are usually strong and lively. Walking and motion could become challenging.
Sleep disorders – Sleep issues can contribute to lack of oxygen due to trouble breathing while asleep. Sometimes, sleep-related symptoms may appear, or they might not show up. But, even if you have sleeping problems, it's best to avoid sleep medication.
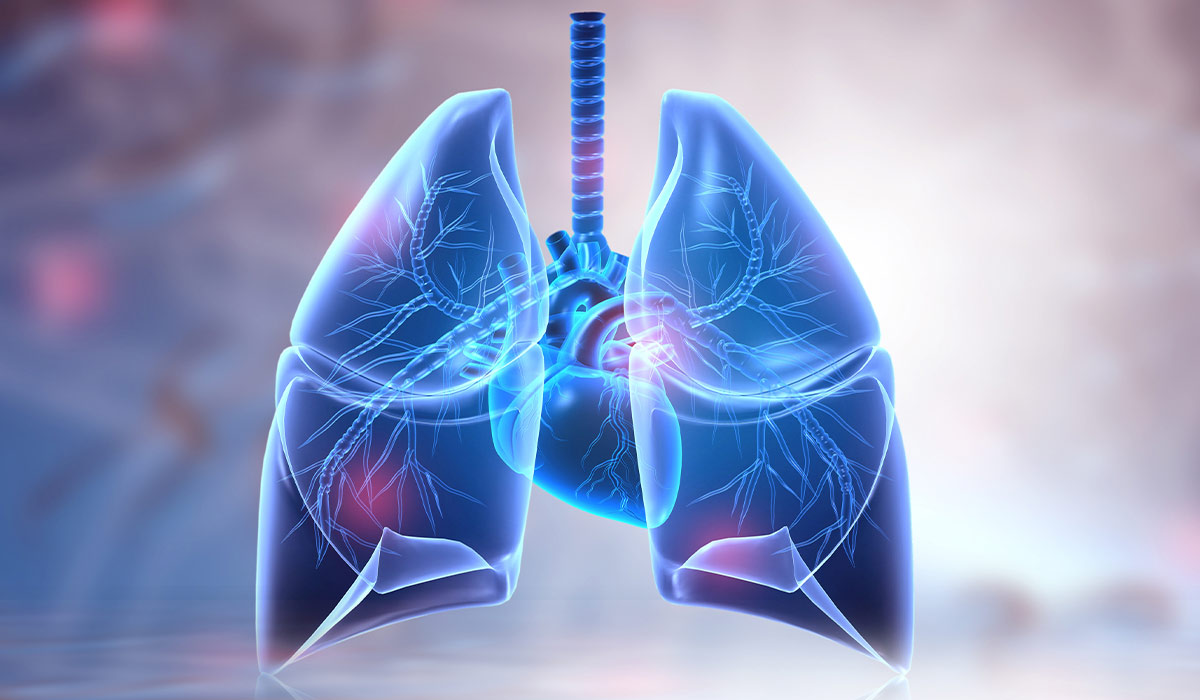
Shortness of breath – In altitude sickness, shortness of breath, dry cough attacks, and difficulty catching your breath may also occur. Severe dyspnoea also persists at rest. When additional symptoms such as cyanosis, accelerated heart rate, and a feeling of tightness in the chest appear, it may indicate High Altitude Pulmonary Edema.
Vomiting – Some patients might struggle with a messed-up appetite and feel nauseous, leading to up-chucking. Altitude sickness often feels like a basic sick feeling, like headaches, feeling dizzy, fever, and throwing up. Some people might feel a little sick, while others could feel very sick. It changes from person to person, based on their unique wellness and readiness. This sickness can seem like other health issues; including tiredness, thirstiness, and being overly cold.
Swelling of the hands, feet and face – Symptoms such as tingling in the limbs, swelling and, in acute cases, cyanosis may also occur. Cyanosis is a hallmark symptom of hypoxia. The disease can cause peripheral oedema, most commonly around the ankles.

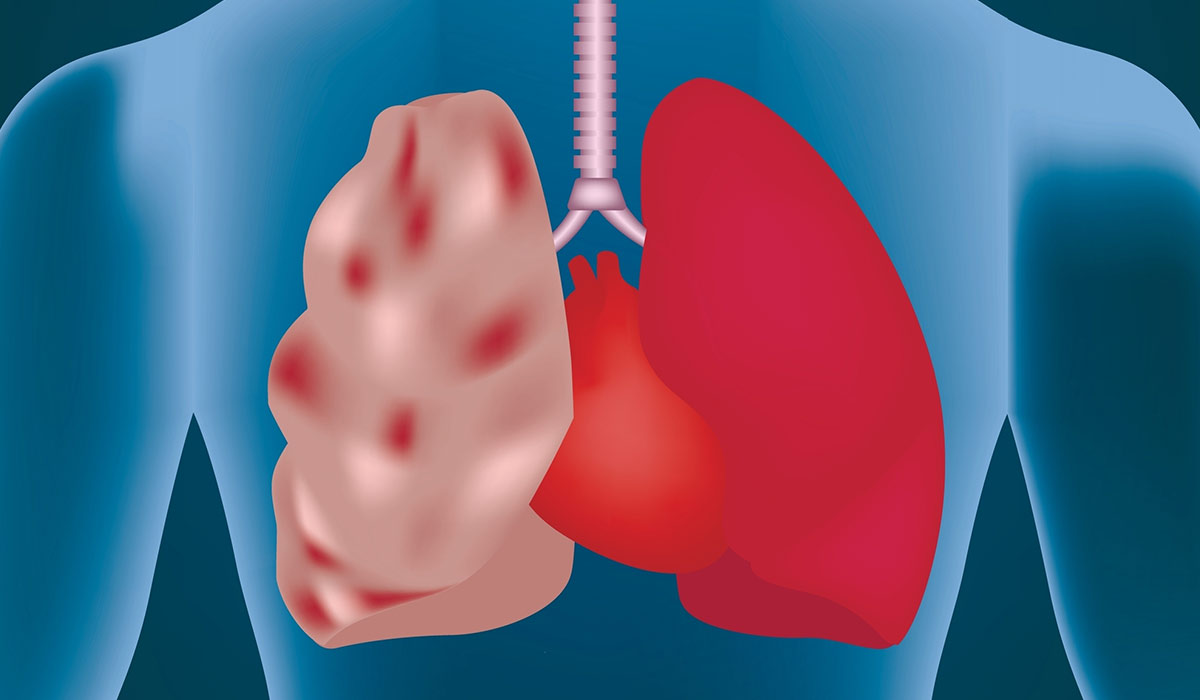
Symptoms occur at very high altitudes above 3,500m. Symptoms of increased acute altitude sickness mean there is a likelihood of cerebral or pulmonary edema. It is then advisable to go lower and seek medical help, as symptoms are life-threatening. High-altitude pulmonary edema's pathophysiology![]() is s an excessive hypoxia-mediated rise in pulmonary vascular resistance or hypoxic pulmonary vasoconstriction leading to increased microvascular hydrostatic pressures despite normal left atrial pressure.
is s an excessive hypoxia-mediated rise in pulmonary vascular resistance or hypoxic pulmonary vasoconstriction leading to increased microvascular hydrostatic pressures despite normal left atrial pressure.
The administration of oxygen, medication, or the use of a hyperbaric chamber only reduces the symptoms. High altitude pulmonary edema is the most common cause of death of all altitude sicknesses, and just after injuries, the second most common cause of death in the mountains. Symptoms include:
Cough – Pulmonary oedema, or fluid in the lungs, brings on sudden symptoms. Short, laboured breaths are common. There's likely to be a cough. At first, the cough is dry. Then it turns wet, producing frothy, pink-hued phlegm.
Cyanosis – When fluid fills the lungs, blood vessels around the body tighten. Limbs may feel cold. Skin may grow a purplish-blue hue, a condition called cyanosis. Often the mouth turns purple. Cyanosis is due to high levels of oxygen-poor blood in the tiny capillaries under our skin.
Accelerated heart rate and breathing – Another sign is a fast heart rate, called tachycardia. The heart normally beats under 100 times a minute. With tachycardia, it beats faster. This can happen with regular or irregular rhythms. Blood pressure might be high or low too.
Chest discomfort – Pain may feel like a press, squeeze, heavy weight, or burn in the chest. If inflammation occurs it may spread, affecting areas such as the shoulders, neck, arms, and belly.

Altitude cerebral edema is a vasogenic edema![]() . This type of atitude sickness is infrequent, statistically affects 1% of people at altitudes above 4,000 m. Treatment is thus like that for altitude pulmonary edema. It is a life- and health-threatening condition, the severity of the symptoms causing coma and subsequent death. Above 5,800 m, complete acclimatisation is impossible and there is a significant risk of altitude sickness. Hypoxia at high altitudes can damage internal organs and lead to death within days. Symptoms of altitude cerebral edema include:
. This type of atitude sickness is infrequent, statistically affects 1% of people at altitudes above 4,000 m. Treatment is thus like that for altitude pulmonary edema. It is a life- and health-threatening condition, the severity of the symptoms causing coma and subsequent death. Above 5,800 m, complete acclimatisation is impossible and there is a significant risk of altitude sickness. Hypoxia at high altitudes can damage internal organs and lead to death within days. Symptoms of altitude cerebral edema include:
Disturbance of consciousness – Disturbance of consciousness is a condition that prevents normal perception of reality and self. Self-control is significantly reduced. Focusing attention can take a lot of work. Emotional disturbances such as anxiety and restlessness may be a symptom of disorders of consciousness. Patients may display aggressive behavior. A person with cerebral edema may appear confused, helpless, and disoriented. A disturbance in the psychomotor drive is not uncommon. Cerebral edema may cause loss of consciousness and coma.
Abnormalities of coordination of body movements – These occur in the character of both slowing down and motor excitation. Movement disorders describe abnormal body movements, such as irregular muscle tone or coordination difficulties, often leading to walking problems.
Hallucinations – Hallucinations are tied to cerebral edema, the brain swelling up due to more permeable blood-brain barrier thanks to low oxygen. This causes strange behavior like irritability, aggression, and irrationality, along with mental confusion. Speaking of confusion, a person may seem wide awake, but their actions and thoughts might not make sense. They could ramble or act weird.
Headache – A notable symptom of cerebral edema is a worsening headache. Cerebral oedema occurs when fluid accumulates in the brain tissue. The pressure inside the skull increases, which can be fatal. Typical symptoms of cerebral oedema include headache, neck stiffness, dizziness, memory, concentration and attention problems, nausea and vomiting, visual problems and seizures.

Treatment depends on the severity of the symptoms and the course of the disease. After the onset of symptoms, you need to rest and stop climbing. It is advisable to rest and avoid physical activity, especially activity that accelerates and deepens breathing. If, despite resting at lower altitude, symptoms persist or worsen at rest, evacuation to an altitude below 1,000 m and medical treatment may be required. Treatments for altitude sickness include:

Thermotherapy – The patient should be protected from hypothermia![]() . Bubble wrap is an excellent insulator, and any dedicated solutions such as heating packs, blankets with heating panels, and thermal blankets, which, by their construction, provide flow and layered insulation, will be suitable for thermal protection of the casualty. If a patient has altitude sickness and lacks suitable items, using extra clothes for warmth is an option.
. Bubble wrap is an excellent insulator, and any dedicated solutions such as heating packs, blankets with heating panels, and thermal blankets, which, by their construction, provide flow and layered insulation, will be suitable for thermal protection of the casualty. If a patient has altitude sickness and lacks suitable items, using extra clothes for warmth is an option.
Oxygen therapy – Oxygen therapy, a method that boosts oxygen concentration![]() in the patient's inhaled air, allows more oxygen to reach lung air sacs, thereby achieving and maintaining normal blood saturations. Oxygen therapy can be passive, with patients breathing in oxygen-rich air through a device, allowing the patient to remain conscious and able to stop therapy when they choose. Active therapy, however, is used in critical situations where the patient might be struggling to breathe independently or is unconscious. This is done with a ventilator. Mountain rescue services usually give oxygen therapy.
in the patient's inhaled air, allows more oxygen to reach lung air sacs, thereby achieving and maintaining normal blood saturations. Oxygen therapy can be passive, with patients breathing in oxygen-rich air through a device, allowing the patient to remain conscious and able to stop therapy when they choose. Active therapy, however, is used in critical situations where the patient might be struggling to breathe independently or is unconscious. This is done with a ventilator. Mountain rescue services usually give oxygen therapy.
Antiemetics – Antiemetics like dimenhydrinate can be used when the patient is throwing up. Rehydration to avoid dehydration, especially for stomach issues, is also critical. Drinking plain water is the most effective way to rehydrate quickly.
Analgesics – RephraseIf a headache happens, either ibuprofen or paracetamol can be used. Avoid using acetylsalicylic acid as it could cause bleeding or worsen stomach ulcers. If after 12 hours, symptoms persist, acetazolamide can be considered.
A***********e – If symptoms do not improve after 12 hours, consider giving a***********e![]() . This medicine increases the frequency and quality of breathing, which means more oxygen enters the body. It reduces the time it takes to get used to it. As well as lowering intraocular pressure, a***********e lowers the pressure in the cerebrospinal fluid by reducing secretion. It also has a diuretic effect, although it is not potent. It increases the excretion of water, potassium sod,ium, and bicarbonate ions.
. This medicine increases the frequency and quality of breathing, which means more oxygen enters the body. It reduces the time it takes to get used to it. As well as lowering intraocular pressure, a***********e lowers the pressure in the cerebrospinal fluid by reducing secretion. It also has a diuretic effect, although it is not potent. It increases the excretion of water, potassium sod,ium, and bicarbonate ions.
N********e – N********e![]() in an extended-release character can be used. A drug's start action happens just 10 minutes after taking it. If symptoms come back, another dose is needed. Without any specific info, more doses depend on each patient's unique situation. It's key to make sure the drug isn't a quick release type. This could cause a big drop in blood pressure.
in an extended-release character can be used. A drug's start action happens just 10 minutes after taking it. If symptoms come back, another dose is needed. Without any specific info, more doses depend on each patient's unique situation. It's key to make sure the drug isn't a quick release type. This could cause a big drop in blood pressure.
D***********e – Dexamethasone![]() is a man-made version of glucocorticosteroid. It's a modified prednisone that has long and strong effects. It reduces swelling, fights allergies, and suppresses your immune system. This drug is used when there's swelling in the brain.
is a man-made version of glucocorticosteroid. It's a modified prednisone that has long and strong effects. It reduces swelling, fights allergies, and suppresses your immune system. This drug is used when there's swelling in the brain.
Portable hyperbaric chamber – A portable hyperbaric chamber![]() is small and easy to carry. It's made to treat serious mountain sickness, swelling in the brain due to high altitude, and fluid in the lungs caused by high altitude. Air gets pushed into the chamber using a manual pump. This makes the pressure inside the chamber go up. The device works by the increase in pressure inside the body. It allows an effect comparable to a descent of approximately 1,500 meters.
is small and easy to carry. It's made to treat serious mountain sickness, swelling in the brain due to high altitude, and fluid in the lungs caused by high altitude. Air gets pushed into the chamber using a manual pump. This makes the pressure inside the chamber go up. The device works by the increase in pressure inside the body. It allows an effect comparable to a descent of approximately 1,500 meters.
The dangerous pathophysiology of altitude sickness calls for preventive measures. Are you planning a skiing, climbing, or trekking trip to the mountains? Make sure you're ready to handle the altitude to avoid getting sick. You need to know your fitness and prepare your body for the changes it will face. This starts long before you hit the trail. Tailor the acclimatization plan individually to each expedition member based on susceptibility to altitude sickness.

The term acclimatization encompasses the slow adaptation of the body to climatic changes: air temperature and humidity, time zone, and altitude-dependent air pressure, which occurs during the first days to weeks of staying in new environmental conditions. Start with a two-night stay above 2,500m at least a month before your trip. This way, your body gets a sneak peek of what's coming. On your first day on the mountain, take it slow. Rest a lot and avoid doing tough tasks. This will help your body adjust. Move up the mountain at a slow, steady pace each day. Climbing up only 300-700 meters each day is a good rule of thumb.
Also, stay hydrated! Water is your best bet. But, you can also choose drinks with low sugar. Aim to drink 2-3 litres a day. You can even go up to 5 litres if you sweat a lot or if you're peeing frequently. Always have water nearby. Eating high-calorie foods![]() will also help. Meanwhile, avoid alcohol and cigarettes. They can harm your body and make it tougher for you to breathe. Don't use them within the first 48 hours of reaching 2,500m. And skip the sleeping pills. They can mess with your breathing and trick you into thinking you slept well.
will also help. Meanwhile, avoid alcohol and cigarettes. They can harm your body and make it tougher for you to breathe. Don't use them within the first 48 hours of reaching 2,500m. And skip the sleeping pills. They can mess with your breathing and trick you into thinking you slept well.
Lastly, remember your meds. A***********e can help prepare your body for the altitude. It should be started a day before you begin your climb. This drug helps your body adjust faster but it can dry you out. So, keep that water bottle handy! Avoid herbal remedies. They may not work. But the most important rule: Listen to your body.
Suit up suitably and take necessary items that will boost your journey and mountain safety. Shield your head and eyes from sun rays to minimize sunstroke chances. Mountains' safety can also be influenced by external elements like altering weather, avalanches, and wilderness creatures. While mapping out a mountain visit, you should bear in mind and get set for all possibilities. Include a helmet, anchoring gear, and different items you might require. This selection might be more or less, depending on the trip nature. By preparing before the trip, following the principles of prevention during the hike, and being aware of possible risks, you can minimize the risk of unpleasant incidents.
Altitude sickness can affect each individual. There are no specific factors, such as age, gender, or physical condition, that increase the risk or likelihood of developing it. The symptoms of altitude sickness occur when you spend some time at altitude, such as skiing or rock climbing. The higher up you are, the more likely it is that they will make themselves known. Altitude sickness is something that people should mainly watch out for:

People with lung disease – The low oxygen levels found at high altitudes can cause various ailments for travelers to high-altitude areas. In high-altitude regions, the air is diluted; the higher you go, the more difficult it is for your body to deliver oxygen to your cells. People with lung disease![]() are prone to increased symptoms of breathlessness. Fast-paced hypoxia happens, causing altitude sickness. Those with lung issues should talk to a doctor who knows about these troubles before going up high.
are prone to increased symptoms of breathlessness. Fast-paced hypoxia happens, causing altitude sickness. Those with lung issues should talk to a doctor who knows about these troubles before going up high.
People with cardiovascular disease – Heart problems can be a worry. Both soaring and low blood pressure can create unease while mountain climbing. People with hypertension are at a higher level of risk of stroke in the mountains, while those with low blood pressure may complain of rapid fatigue and dizziness on the trail. For this reason, people in this group should also seek specialist medical advice before venturing into the high-altitude mountains.
People with diabetes – Diabetics don't have a higher chance of getting altitude sickness than others. But, they need to know that altitude sickness can cause diabetes complications which may be tricky to manage.
Pregnant women – Going to high elevations is not typically ill-advised for pregnant women. Before embarking on trips to high altitude, they should speak to a doctor. High elevation carries risks of low oxygen and miscarriage. In its initial stage, pregnancy can manifest symptoms of sluggishness and nausea, which could add difficulty to such journeys. Moderation of physical activity is also recommended during pregnancy.
Children – The children attack rate![]() appears similar to that in adults. Still, high-altitude trips can be strenuous for kids, thus necessitating consideration of each child's individual abilities. It's important to remember that babies and small children have a higher risk of hypothermia and frostbite due to their ratio of body surface area to weight. In addition, a child carried by a parent does not generate heat with its muscles. Children's skin is more susceptible to sunburn. In children under the age of three, any change in environment can cause disturbances in sleep, appetite, activity and mood, making it difficult to recognise the symptoms of altitude sickness.
appears similar to that in adults. Still, high-altitude trips can be strenuous for kids, thus necessitating consideration of each child's individual abilities. It's important to remember that babies and small children have a higher risk of hypothermia and frostbite due to their ratio of body surface area to weight. In addition, a child carried by a parent does not generate heat with its muscles. Children's skin is more susceptible to sunburn. In children under the age of three, any change in environment can cause disturbances in sleep, appetite, activity and mood, making it difficult to recognise the symptoms of altitude sickness.
The occurrence of altitude sickness can be observed in healthy but poorly acclimatized people who travel to an altitude of more than 2,500 meters above sea level in a short time. The first symptoms appear after only 6 hours. We may then notice a headache, vomiting, nausea, or insomnia. These disorders are caused by too little oxygen being supplied to the body. Thus, the body has yet to adapt to such a high altitude, and the tolerance zone has been exceeded. Mountain sickness is caused by low oxygen pressure in the inhaled air.
As a consequence of the body's maladaptation to high altitude conditions, acute mountain sickness often occurs with its primary and most serious complications: high altitude cerebral edema and pulmonary edema. There are various methods of treating altitude sickness used by mountain rescuers. The acclimatization process must be planned and properly graded to reduce the risk of altitude sickness. It is a type of adaptation to a new location, where the body adjusts to the new conditions.
Table of Contents

Cerebral palsy is a set of disorders characterized by impaired psychomotor development. What are its causes? What is the treatment… read more »
Do you know what are the symptoms of edema? How is it treated? Do you need a special diet if… read more »

A pulmonary embolism develops when a clump, most often a blood clot, gets stuck inside the lung blood vessel. It… read more »

Hypoxia occurs when the body's tissues don't get enough oxygen. Suffering from this issue can lead to breathing difficulties, an… read more »
Hypercapnia is a condition in which the partial pressure of carbon dioxide in our blood is increased. This can be… read more »

Aneurysm refers to an abnormal swelling in a blood vessel. It is also known as a brain aneurysm, cerebral aneurysm,… read more »

Swollen feet is an outward sign of fluid accumulation in the body. It can be a symptom of serious health… read more »

Pneumothorax is a condition that develops as a result of air entering the pleural cavity. What are the causes and… read more »
Emphysema is a lung disease that involves excessive aeration of the lungs, which disrupts gas exchange in the body. How… read more »