Periodontitis, or periodontal disease, is a serious gum disease caused by bacteria, leading to inflammation of soft tissues around your teeth. If left untreated, periodontitis may damage and even destroy the structures that support the teeth.
Periodontitis can be prevented in its early stages. However, it can't be cured if it progresses to advanced stages, which cause significant damage to the bones and teeth.
Continue reading the article to learn about the four stages of periodontitis, its causes, risk factors, available treatment strategies, and ways to prevent this condition from developing.
According to the report by the Centers for Disease Control and Prevention (CDC), 47.2% of adults in their 30s and older are affected by one of the stages of periodontitis, which makes it a very common condition. CDC notes that the number of people with this condition increases with age. It is estimated that as much as 70.1% of adults above 65 years old have this disease.
Periodontitis is considered a severe and potentially dangerous condition. At an advanced stage, periodontal disease involves inflammation and infection of the structures supporting the teeth, including the gums, periodontal ligament, and alveolar bone. If left untreated, periodontitis can lead to various complications and pose risks to oral and overall health.
A primary cause of periodontitis is usually anaerobes such as Treponema denticola and Porphyromonas gingivalis![]() . These bacteria are only a tiny fraction of bacteria types that normally live in a human mouth. A healthy person's mouth has hundreds of various kinds of bacteria, most of which don't threaten oral health. However, if you don't take proper care of your teeth, gums, and mouth, you risk being affected by some bacteria, such as Treponema denticola and Porphyromonas gingivalis.
. These bacteria are only a tiny fraction of bacteria types that normally live in a human mouth. A healthy person's mouth has hundreds of various kinds of bacteria, most of which don't threaten oral health. However, if you don't take proper care of your teeth, gums, and mouth, you risk being affected by some bacteria, such as Treponema denticola and Porphyromonas gingivalis.
Early periodontitis happens when harmful bacteria grow and multiply on your teeth. It can be normally prevented by daily oral care, including brushing your teeth, flossing, and using mouthwash. If your teeth are left unattended for a long time, the bacteria can form a plaque – a sticky deposit of bacteria.
There are four stages of periodontitis: inflammation (gingivitis), early periodontal disease, moderate periodontal disease, and advanced periodontal disease. If diagnosed at its early stages, periodontitis is easier to treat than moderate and advanced periodontitis, which may require surgery. Let's take a closer look at how the disease develops:
Periodontitis is typically preceded by gingivitis![]() , an early-stage gum disease that is significantly less severe and problematic. Gingivitis causes similar symptoms to periodontitis:
, an early-stage gum disease that is significantly less severe and problematic. Gingivitis causes similar symptoms to periodontitis:
However, unlike periodontitis, gingivitis does not damage and destroy the bone around the teeth and is usually reversible if you take better care of your teeth. It can also be treated with regular professional dental cleanings.
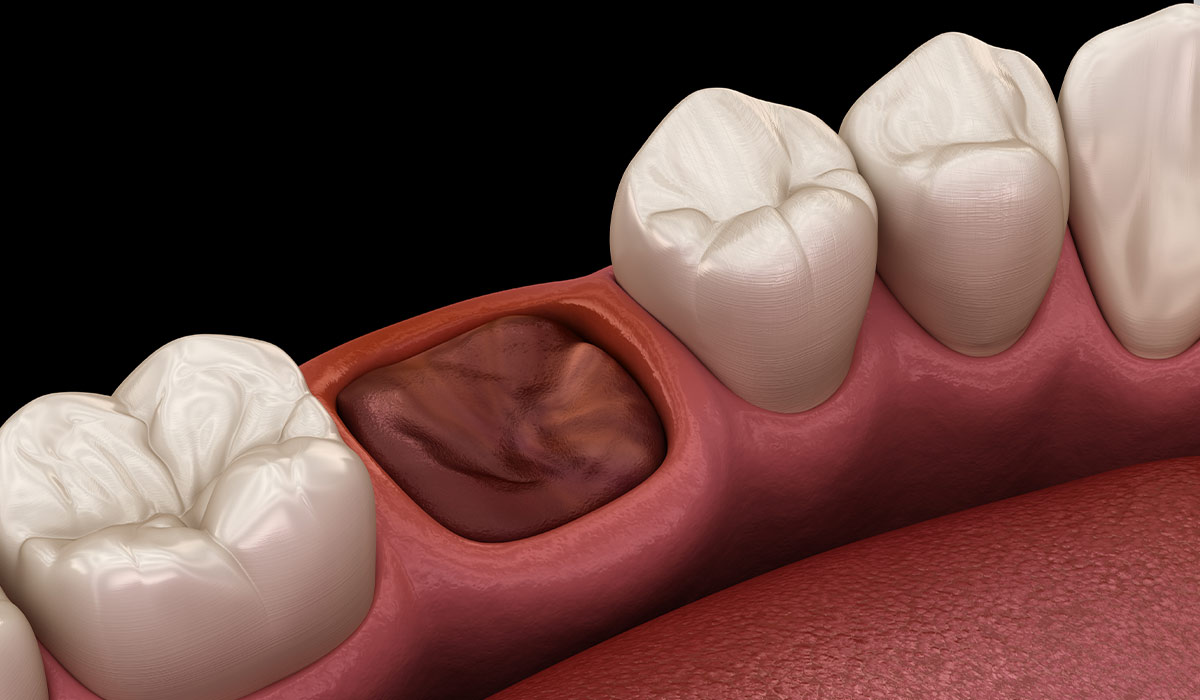
If gingivitis is left untreated, it can progress to the second stage – early periodontal disease, also referred to as slight or mild. The telltale signs of this stage are gums pulling away from the teeth, loss of bones around the gums, and periodontal pockets – openings surrounding the teeth. Plaque and bacteria may get trapped inside these spaces and can no longer be reached with a toothbrush or floss.
As it is difficult to stop mild periodontal disease with better oral care, it often progresses to the third stage, called moderate periodontal disease. At this stage, an affected individual loses more bone around the gums, making them tender and swollen.
Without treatment, periodontal disease eventually progresses to the last stage, known as advanced periodontal disease. Characteristic signs of this stage are painful abscesses, tooth loss, bleeding gums, pus around the gum line, and chronic bad breath.
Factors that are associated with an increased risk of periodontitis include:

Symptoms caused by periodontitis depend on the stage of the disease but commonly include the following health problems:
In its early stages, periodontitis may not cause any noticeable health issues. It may not cause any pain and keep developing without any apparent signs. In many cases, only a dentist can tell if you have periodontitis, even if it has progressed to the late stage. To diagnose this disease early, it is important to always pay attention to any changes in your oral health, such as blood on your toothbrush after brushing, persistent bad breath, and changes in how your gums feel and look. If you spot such issues, schedule an appointment with your dentist as soon as possible to avoid any potential complications of periodontitis.
If left untreated, periodontitis can damage structures that support your jaw. As a result, your teeth may loosen and fall out or require surgical removal. In addition, it may lead to painful abscesses, receding gums that expose your teeth, and migration of teeth.
Moreover, if the bacteria responsible for periodontitis enters your bloodstream through the gum tissue, it can affect other body parts. If that happens, the following complications may occur:
Based on the visible symptoms, dentists can usually tell if a person has periodontitis, gingivitis, or other gum disease. Telltale signs of gum issues, such as gum bleeding, plaque, and tartar buildup, are often spotted during a routine dental examination or while diagnosing another dental issue.
If your dentist suspects periodontitis, they will ask you about your symptoms, when they started, and whether they got worse. They will also review your medical history to determine if there are factors that may have led to the development of gum disease.
In addition, you may be asked to have a dental X-ray to check for bone loss and an additional visit to a gum disease specialist (periodontist) for further assessment.
Based on the diagnosis, you will be assigned a grade of periodontitis and presented with treatment options that would work best for your case.
Treatment strategies for periodontitis depend on the severity of the disease. Mild and moderate gum diseases are usually treated with non-surgical methods, including antibiotics, scaling, and root planning. Severe periodontitis often requires surgical intervention, including gum grafts, dental bone grafts, guided tissue regeneration, flap surgery, and other procedures.
Topical and oral antibiotics are often prescribed to control bacterial infection. These usually include antibiotic gels underneath the gums, antibiotic mouth rinses, and oral antibiotics.
Scaling is a procedure in which tartar and bacteria are removed from the tooth surface and beneath the gumline. The procedure can be performed with an ultrasonic device or laser.
The root planing procedure aims to smooth the root surface to prevent bacteria buildup. The procedure also helps the gums attach themselves to the teeth.
One of the most problematic issues caused by periodontitis is gum recession, which occurs when gum tissue pulls away from the teeth. This problem can be resolved with a gum graft, a surgery that helps restore lost tissue around the teeth.
In this procedure, a dentist or periodontist attaches a tissue graft to the affected place. The donor tissue can be obtained from the roof of the patient's mouth or purchased from a licensed tissue bank. The surgery helps reduce further gum loss, improves the appearance of the teeth, and covers the exposed teeth roots.
A periodontist or dentist may recommend dental bone grafts in cases of significant bone loss. The procedure involves placing bone-grafting material in areas that lost bone tissue. A material can be obtained from the patient's bone or tissue bank. In some cases, a graft can be synthetic.
The bone graft procedure aims to reduce the risk of further tooth loss and prevent infections. The graft also allows a new bone to grow and keep the teeth in place.
Guided tissue regeneration![]() is when a healthcare professional places a biocompatible membrane between the tooth and existing bone. This prevents the tissue from growing in this area, promoting the growth of a bone instead.
is when a healthcare professional places a biocompatible membrane between the tooth and existing bone. This prevents the tissue from growing in this area, promoting the growth of a bone instead.
Also called pocket reduction surgery, flap surgery is a procedure that involves cutting the gums to lift the gum tissue away from the teeth temporarily. This exposes teeth roots and allows a periodontist to plan scaling or root.
Platelet-rich plasma is a procedure that helps regenerate lost bone or gum tissue. To perform it, a dentist or periodontist obtains platelet-rich plasma from a sample of a patient's blood and then spins it in a centrifuge to separate plasma from blood cells. The plasma is then placed in areas lacking bone or gum to stimulate new tissue growth.
Outlook for periodontitis is usually optimistic for stages I and II![]() , where it can be treated with proper oral care at home or with professional dental cleanings. The disease becomes more challenging to treat at stages III and IV (moderate and advanced periodontitis, respectively) because it requires a personalized treatment strategy, including one or more of many available procedures or surgery in the most severe cases.
, where it can be treated with proper oral care at home or with professional dental cleanings. The disease becomes more challenging to treat at stages III and IV (moderate and advanced periodontitis, respectively) because it requires a personalized treatment strategy, including one or more of many available procedures or surgery in the most severe cases.
Unfortunately, there is no cure for severe periodontal disease, but it can be managed with an adequate maintenance plan, oral hygiene, procedures, and medications.
Preventing periodontitis involves good oral hygiene practices and making healthy lifestyle choices. Here are some tips to help prevent periodontitis:

Periodontitis, or periodontal disease, is a severe gum disease caused by bacterial inflammation that can damage and destroy structures supporting teeth.
The disease progresses through four stages: inflammation (gingivitis), early periodontal disease, moderate periodontal disease, and advanced periodontal disease. Early detection in the inflammation stage allows for a more positive outlook.
Signs and symptoms of periodontitis include bad breath, bleeding gums, pain while chewing, swollen and receding gums, loose or shifting teeth, and pus between gums and teeth. Complications can lead to tooth loss and may affect overall health, contributing to conditions like diabetes, heart disease, and respiratory issues.
Treatment varies with disease severity. Mild to moderate cases can be treated with non-surgical methods such as antibiotics, scaling, and root planning. Severe cases may require surgical interventions like gum grafts, dental bone grafts, guided tissue regeneration, and flap surgery.
Prevention is vital and involves regular brushing with fluoride toothpaste, daily flossing, using an antiseptic mouthwash, avoiding tobacco, managing stress, and attending regular dental check-ups. Periodontitis prognosis is optimistic for early stages but becomes more challenging in advanced stages, necessitating personalized treatment plans.
Table of Contents
Periodontal Disease is a notorious dilemma of swelling in the tissues around teeth, ordinarily due to plaque buildup—a sticky layer… read more »
Gingivitis is a very common condition affecting the gums. It is a mild form of gum disease that causes bleeding… read more »

A toothache is an unpleasant symptom that can have various causes. Learn methods on how to deal with a toothache,… read more »

An abscess tooth is a painful dental condition characterized by a pocket of pus that forms due to a bacterial… read more »

Bad breath is a common problem that can reduce quality of life. Find out the most common causes of halitosis… read more »

Ehlers-Danlos Syndrome is a group of diseases with a genetic basis. Learn all the symptoms associated with EDS. Find out… read more »
A dry socket may occur after tooth extraction, a procedure in which a tooth is removed from the socket in… read more »
Bone cancer is a disease in which cancerous lesions develop in bone tissue. It can be primary or a result… read more »

Leukoplakia is a disease that most commonly affects the oral cavity. A complication of leukoplakia can be cancer, so it… read more »