An abscess is a circumscribed cavity containing purulent material. This condition arises due to the degradation and liquefaction of dead tissues, which occurs due to the action of cellular enzymes such as proteases, lipases, or oxidases.
Typically, an abscess forms due to an advanced carious process that culminates in inflammation and necrosis of the tooth pulp. The necrotic pulp provides a conducive environment for the proliferation of pathogens that penetrate the periapical tissues, leading to acute, purulent inflammation of the tooth.

There are two basic types of abscesses: abscess gum and abscess tooth.
A gum abscess, also known as a periodontal abscess![]() , is caused by an infection of the area between the gum and the tooth. The infection may result from excessive accumulation of dental plaque or advanced periodontal disease.
, is caused by an infection of the area between the gum and the tooth. The infection may result from excessive accumulation of dental plaque or advanced periodontal disease.
An abscess tooth forms at the tip of the root. It occurs when the contents of the root canal die.
Depending on the severity, spread, and size of abscesses, there are three basic types of tooth abscess:
Pus in the gum is a typical symptom of inflammation, usually developing as a result of deep carious lesions and bacterial infection, but not only that.
The most common causes of the dental abscess![]() include:
include:
Inflammation of periapical tissues with the subsequent formation of an abscess tooth![]() may have many causes; specialists divide them into two groups for convenience: infectious and non-infectious.
may have many causes; specialists divide them into two groups for convenience: infectious and non-infectious.
Bacterial infections are the most common source of pathology in the tissues around the root apex. They cause both acute and chronic inflammation.
The death of the pulp, the innermost part of the tooth that is highly vascularized and innervated, can result in gangrenous necrosis, which is susceptible to bacterial superinfection. Upon entering the damaged pulp, microorganisms multiply rapidly, producing toxins that exacerbate the condition. The body responds by initiating local inflammation to defend itself against the infection.
Pathogenic microorganisms continue to penetrate from the pulp, through the root canal, and into the periapical tissues. The influx of immune system cells initially results in an inflammatory infiltrate, which ultimately develops into an abscessed tooth.
Bacterial infiltration of the pulp primarily occurs through carious lesions that allow microorganisms to penetrate the tooth's interior. Therefore, a dentist must promptly treat even minor cavities to prevent![]() infection and abscess tooth formation.
infection and abscess tooth formation.
Other places that serve as portals for bacteria to enter the tooth chamber include:
Non-infectious causes of periapical inflammation include mechanical, chemical, thermal, autoimmune injuries, and pulpitis.
Many of them are adverse events following improperly or unskillfully performed dental procedures. Complications that arise from contact with health care are called iatrogenic. Non-infectious inflammations may be related to puncturing the tissues around the root apex or manipulations that are too violent during orthodontic or root canal treatment.
Substances previously used to destroy the pulp were the cause of chemical inflammation. It is worth remembering that after superinfection with pathogenic microorganisms, non-infectious inflammation may turn into bacterial inflammation, which is only a step toward abscess tooth formation.
The appearance and intensive multiplication of bacteria in the root canal is the most common cause of the development of an abscessed tooth. The body responds to the invasion of microorganisms with local inflammation. Due to the degree of advancement of the changes and the symptoms![]() presented, the following are distinguished:
presented, the following are distinguished:

In the case of a periapical abscess![]() , an acute and intense pain in the tooth becomes prominent. The pain is often spontaneous, continuous, or aggravated by pressure or biting. Increased warmth and a horizontal body position exacerbate these unpleasant symptoms.
, an acute and intense pain in the tooth becomes prominent. The pain is often spontaneous, continuous, or aggravated by pressure or biting. Increased warmth and a horizontal body position exacerbate these unpleasant symptoms.
The current swelling of the surrounding tissues may lead to temporary deformation of the facial features—blood flow over the affected area increases, accompanied by a local feeling of heat. The affected tooth reacts painfully when tapped and may display multiple carious lesions and discoloration.
A subperiosteal abscess![]() is characterized by similar but more severe symptoms. General symptoms, such as fever, chills, or feeling unwell, are often present.
is characterized by similar but more severe symptoms. General symptoms, such as fever, chills, or feeling unwell, are often present.
The last stage is characterized by the penetration of the abscessed tooth into the soft tissues, which reduces pain and increases swelling of the surrounding tissues.
An abscessed tooth, characterized by chronic inflammation of the periapical tissues, can manifest without or mild symptoms. In such cases, a thorough diagnosis and implementation of appropriate therapy are of utmost importance.
Failure to address a dental infection can result in the spread of microorganisms to other oral tissues and the transmission of bacteria into the bloodstream, which can lead to severe diseases such as infective endocarditis, pneumonia, arthritis, and sepsis. It is, therefore, significant to seek timely and effective treatment to prevent such complications from developing.
In some cases, the abscess tooth ruptures independently and releases pus. Sometimes, a fistula appears on the gum, i.e., a tiny opening or bubble through which pus is released. The appearance of a fistula indicates a long-term inflammatory process.
Remember that bursting the follicle and releasing pus does not solve the problem. It is only a sign of inflammation in the periodontium, which necessarily requires the intervention of a dentist.
An abscessed tooth is a severe condition that necessitates professional intervention and is not amenable to self-treatment using only home remedies. The inflammatory process can propagate through blood and lymphatic vessels to distant organs, causing odontogenic infections that pose a significant health hazard. As a result, specialized dental care is essential to halt the progression of an abscess.
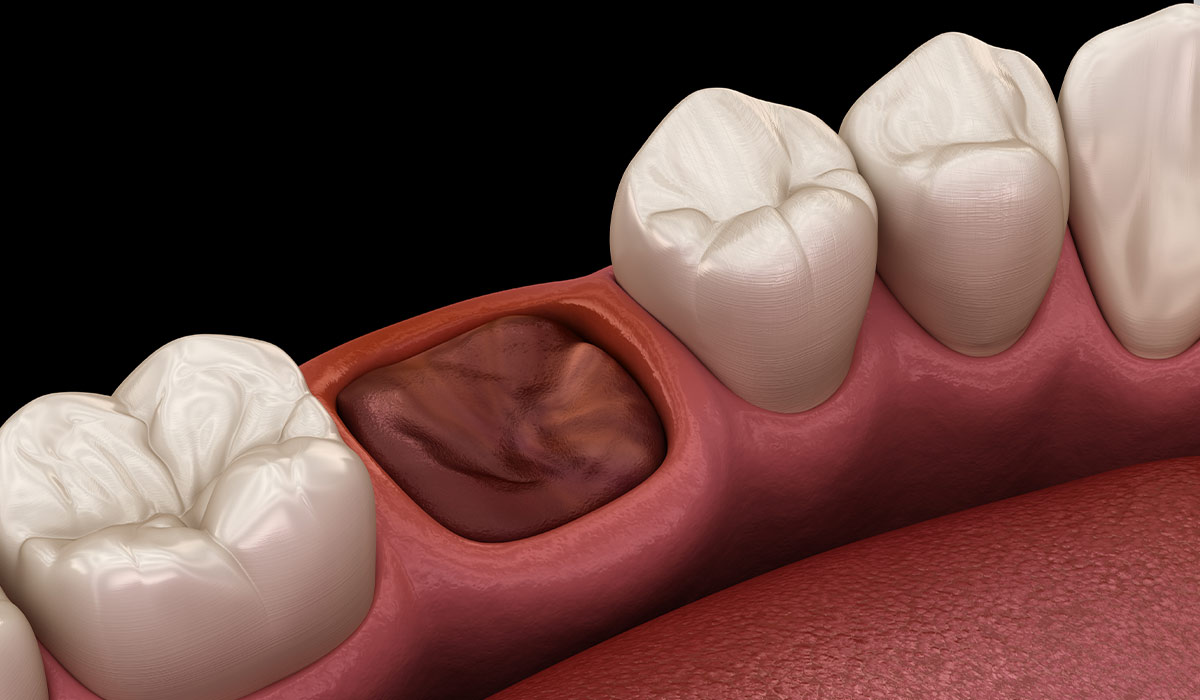
An apical abscess is a chamber that develops in the bone at the apex of the tooth root and is filled with pus. The most prevalent cause of apical abscess is untreated caries, which leads to pulp diseases. Necrosis, gangrene, and pulp inflammation are pathological manifestations of the pulp disease.
For an abscess to form, bacteria must be present in the tooth canals, which happens in the case of pulp necrosis or gangrene. Another reason for the development of an abscess may be the failure of root canal treatment, which results from, among others, not finding all the canals in the tooth, insufficient rinsing and disinfection, or superinfection of the canals as a result of leaky tooth reconstruction after completed root canal treatment.
An abscess tooth develops in several stages, from a periapical abscess to a subperiosteal abscess to a submucosal abscess.
During the initial phase of a tooth root infection, inflammation affects the surrounding tissues. A key indicator of this stage is intense, throbbing pain, exacerbated by lying down, changes in temperature, and biting. The discomfort may spread to the ear, jaw, or neck, and the patient may report a sensation of the tooth becoming dislodged from its socket.
The subperiosteal abscess stage, considered the most acute stage of inflammation, is characterized by the penetration of purulent exudate into the periosteum through the bone. The pain becomes more severe during this stage and may radiate to other teeth. Additionally, the gum becomes visibly red and swollen, and the patient may experience a slight increase in body temperature.
The last stage – submucosal abscess – occurs when the purulent exudate penetrates under the mucosa. Pus often spontaneously releases into the mouth, which causes an unpleasant smell and taste. Although in this phase, the pain may stop, the swelling of the gums increases, and the tissues around the abscess become warm and red. General symptoms, such as fever or malaise, are also possible. The rupture of an abscess does not mean the end of the problem, as the inflammatory process may continue to progress due to bacteria in the abscess cavity.
However, the developing inflammation in the bone may be asymptomatic for a long time and is often detected accidentally during routine radiological examinations, e.g., after a panoramic radiograph.
If there is a suspicion of an abscess, prompt dental attention is crucial. The dentist will likely perform an incision in the abscess to remove any remaining pus, irrigate the abscess cavity to eliminate bacteria as much as possible, place drains to drain any remaining pus, and may also prescribe appropriate medications. It is a temporary measure, but the most crucial aspect in treating purulent inflammation is identifying the cause of the abscess and treating the causative tooth. It may entail root canal treatment or, in some cases, tooth extraction.
Antibiotics![]() are employed when systemic symptoms such as fever are present and prophylactically in patients with weakened immunity, systemic illnesses, who have undergone transplants, or who are taking various medications. However, antibiotics are not always necessary to manage an abscess tooth.
are employed when systemic symptoms such as fever are present and prophylactically in patients with weakened immunity, systemic illnesses, who have undergone transplants, or who are taking various medications. However, antibiotics are not always necessary to manage an abscess tooth.

Home remedies can only provide temporary relief, but you should see a dentist as soon as possible.
Cold compresses![]() on the swollen area have a soothing effect and will reduce swelling and pain.
on the swollen area have a soothing effect and will reduce swelling and pain.
Rinsing your mouth with a solution of water and salt![]() has a bacteriostatic effect, which means it limits the growth of bacteria; it should be done several times a day.
has a bacteriostatic effect, which means it limits the growth of bacteria; it should be done several times a day.
A baking soda solution can reduce swelling and “draw out” pus that escapes through the gum.
Chamomile infusion has a soothing effect, it is worth rinsing your mouth with the cooled infusion to relieve pain.
Sage decoction has anti-inflammatory and disinfecting properties, so it can be useful in alleviating the symptoms of abscess teeth. There are ready-made herbal rinses that you can buy at a pharmacy.
Painkillers![]() or anti-inflammatory drugs (NSAIDs) may also be helpful. They can be obtained without a prescription and should be used according to the leaflet. However, only dental treatment will help to eliminate the problem.
or anti-inflammatory drugs (NSAIDs) may also be helpful. They can be obtained without a prescription and should be used according to the leaflet. However, only dental treatment will help to eliminate the problem.
If left untreated, an abscess tooth can cause several serious complications![]() . The most frequently observed:
. The most frequently observed:
Pain is one of the most characteristic symptoms of an abscess tooth. It usually worsens when lying down, which is why patients often describe it as “night pain.” It may make it difficult to fall asleep and disturb sleep continuity.
Untreated abscesses, accompanied by a pervasive inflammatory process, may lead to complications such as difficulty opening the mouth or breathing problems. They significantly impede the performance of physiological activities and pose a threat to health.
If any symptom or a significant deterioration of the patient's general condition happens, you should immediately see a dentist.
Table of Contents

A toothache is an unpleasant symptom that can have various causes. Learn methods on how to deal with a toothache,… read more »
Periodontal Disease is a notorious dilemma of swelling in the tissues around teeth, ordinarily due to plaque buildup—a sticky layer… read more »

An abscess is a pocket of pus that emerges when bacteria cause an infection, leading to swelling in the organism's… read more »

Periodontitis, or periodontal disease, is a serious gum disease caused by bacteria, leading to inflammation of soft tissues around your… read more »
Gingivitis is a very common condition affecting the gums. It is a mild form of gum disease that causes bleeding… read more »
A dry socket may occur after tooth extraction, a procedure in which a tooth is removed from the socket in… read more »
Mastitis is a condition that can affect many women, especially during the postpartum period. What symptoms does it cause? What… read more »
Necrosis refers to the death of cells constituting a body tissue. Dead or necrotic tissue can occur when blood supply… read more »

Bad breath is a common problem that can reduce quality of life. Find out the most common causes of halitosis… read more »