Huntington's Disease is a genetically based neurological condition of the nervous system. The disease is genetically determined in an autosomal dominant manner. Its exact cause is the presence of a specific gene. Symptoms of the condition usually appear in patients between 30 and 50.
In the course of the disease, the main symptoms are so-called choreic movements, dementia, and personality disorders. Usually, the onset of Huntington's chorea is barely noticeable, and the symptoms worsen over time.
The course of the disease is progressive and leads to irreversible changes in the brain. The first element necessary for a correct diagnosis of Huntington's Disease is a thorough medical history. Examining the presence and severity of all symptoms according to diagnostic criteria is essential. Next, neurological tests, imaging studies, or genetic tests may be necessary.
Huntington's disease cannot be cured entirely, but it is possible to alleviate symptoms to make the patient's life more comfortable. There are various forms of pharmacotherapy to ease the symptoms of Huntington's Disease. Research is currently underway to find an effective treatment for the disease. In addition, multiple associations are helping to organize rehabilitation, medical care, financial, and psychological support for patients and their families.
Huntington's disease (HD) is an illness caused by the Huntingtin Gene (HTT)![]() . Mutation of this gene leads to neurodegeneration. Mutated huntingtin causes damage to the neurons of the central nervous system. Huntington's disease patients have an increased number of CAG trinucleotide
. Mutation of this gene leads to neurodegeneration. Mutated huntingtin causes damage to the neurons of the central nervous system. Huntington's disease patients have an increased number of CAG trinucleotide![]() repeats. The more these nucleotides repeat, the earlier and more severe the disease symptoms will appear.
repeats. The more these nucleotides repeat, the earlier and more severe the disease symptoms will appear.
The HTT gene was discovered in 1993. This discovery makes it possible to test people at risk of HD. Confirmation of the Disease is possible through DNA testing. Inheritance is gender-independent, meaning both men and women are at the same risk. The disease is inherited from one parent. In addition to genetic factors, attention is drawn to other factors whose influence still needs clarification. These factors include environmental elements![]() or modifying gene factors
or modifying gene factors![]() .
.

The disease most commonly affects patients between the ages of 30 and 50![]() , but there are also cases of the juvenile form, which can occur even before the age of 20. Disorders of the central nervous system characterize Huntington's Disease. The prevalence of Huntington's Disease worldwide varies by geographical area. Huntington's disease is a rare condition with a prevalence of 2.7 per 100,000
, but there are also cases of the juvenile form, which can occur even before the age of 20. Disorders of the central nervous system characterize Huntington's Disease. The prevalence of Huntington's Disease worldwide varies by geographical area. Huntington's disease is a rare condition with a prevalence of 2.7 per 100,000![]() worldwide.
worldwide.
Huntington's disease is categorized into several stages that characterize a patient's functional capacity. The scale includes stages 1 to 5. The earliest stage indicates the early stage of the disease when the patient can fully function. The last stage, on the other hand, identifies patients who require total care and are most often in a nursing home.
The main feature of Huntington's Disease is neuronal degeneration, which is the cause of the symptoms that occur and progress over time. Huntington's disease symptoms can be divided into three groups: motor![]() , cognitive
, cognitive![]() , and psychiatric
, and psychiatric![]() . Motor symptoms usually develop slowly, starting with a slight degree. Cognitive impairment occurring at first may also be limited and challenging to pick up. In contrast, psychiatric symptoms may include a variety of signs. They are most commonly associated with frontal lobe function. The presence of psychiatric symptoms requires specialized care to maintain mental health.
. Motor symptoms usually develop slowly, starting with a slight degree. Cognitive impairment occurring at first may also be limited and challenging to pick up. In contrast, psychiatric symptoms may include a variety of signs. They are most commonly associated with frontal lobe function. The presence of psychiatric symptoms requires specialized care to maintain mental health.
Motor disorders are the first symptoms that may prompt a patient to see a doctor. Motor disorders are a group of symptoms that have in common abnormalities in body movements, muscle tone, and the ability to coordinate complex activities. Such symptoms present in Huntington's Disease include:
In Huntington's Disease, motor symptoms refer to involuntary movements that initially start from the limbs but may also affect the facial muscles. The movements gradually spread and increase in intensity as the disease progresses. The motor symptoms are described as chorea![]() , which is related to the fact that Huntington's Disease used to be called Huntington's chorea.
, which is related to the fact that Huntington's Disease used to be called Huntington's chorea.
Chorea is a movement disorder characterized by continuous, fluid, but abnormal movements accompanied by decreased muscle tone. The choreic movements are often exacerbated by the arbitrary movements that the patient attempts. Patients cannot control their motor symptoms, which affects their performance in daily activities. Patients in the late stage of the disease are unable to dress themselves and move in a wheelchair.
Apraxia is a neurological disorder that causes an inability or difficulty performing familiar activities. It is associated with damage to the great spiracle and sometimes to precentral structures in the frontal lobes. Neurodegeneration causes problems with the transmission of information between neurons that are responsible for motor skills. Apraxia is divided into several types. In Huntington's Disease, hypotonic-hyperkinetic apraxia is characterized by decreased muscle tone with increased involuntary movements.
This symptom is rare in Huntington's Disease but can occur along with other motor symptoms. Ataxia is a neurological symptom involving a lack of voluntary coordination of muscle movements, including gait abnormalities, speech changes, and eye movement abnormalities. Ataxia is a clinical sign that sections of the nervous system that are in charge of movement, such as the cerebellum, are not working properly. Ataxia, therefore, leads to symptoms such as postural abnormalities![]() , gait abnormalities
, gait abnormalities![]() , and eye movement abnormalities
, and eye movement abnormalities![]() .
.
Neurological diseases often lead to a change in the way patients walk. At an early stage, patients with Huntington's Disease may experience gait wobble. Walking becomes increasingly complex, and patients appear clumsy. Patients cannot control unexpected, involuntary body movements; their gait becomes ‘dance-like,' with characteristic side-to-side swaying. In the late stages, HD patients are unable to move independently and are bedridden or use wheelchairs.
Uncontrolled eye movements also occur in association with ataxia. Patients show slow eye movements, resulting in dysfunctional gaze. These involuntary eye movements are described as nystagmus. With nystagmus, the eyes cannot be focused on the selected image, and vision is disturbed and blurred.

Bradykinesia is a symptom denoting motor slowing. It is characteristic of Parkinson's Disease but also occurs in Huntington's Disease—bradykinesia, which results in slower performance of all activities. Patients are slower to dress, walk, and speak. They have difficulty starting a movement and speeding it up. Bradykinesia is often accompanied by a gradual worsening of symptoms that initially makes it difficult and, over time, can completely prevent independent functioning. Motor slowing takes its extreme form in a complete inability to make conscious movements.
Dystonia is also included in the group of movement disorders found in Huntington's Disease. Involuntary movements and postural disturbances characterize it. Dystonia can affect one part of the body or several different parts. The involuntary movements cause the bending and twisting of various body parts, leading to an unnatural posture. After years of the disease, the abnormal body positioning becomes fixed. As the disease progresses, dystonia may involve new parts of the body not previously affected by involuntary movements.
Babinski's sign occurs in HD and other conditions. Babinski's reflex![]() in neonates, infants, and young children is a physiological, normal response of the body regarding nervous system function, whereas that observed in adults represents a pathological situation requiring neurological examination. The reflex is triggered by foot irritation in the lateral basal area. Babinski's sign consists of an isolated movement of the toe extensor due to irritation. Patients bend the big toe towards the top of the foot while visiting the other toes upwards.
in neonates, infants, and young children is a physiological, normal response of the body regarding nervous system function, whereas that observed in adults represents a pathological situation requiring neurological examination. The reflex is triggered by foot irritation in the lateral basal area. Babinski's sign consists of an isolated movement of the toe extensor due to irritation. Patients bend the big toe towards the top of the foot while visiting the other toes upwards.
Dysarthria is categorized as a speech disorder that occurs in the course of neurological diseases. Dysarthria is one type of speech disorder associated with a motor disorder. It involves an inability to coordinate the muscles used to produce speech, namely the muscles of the face, mouth, or respiratory system. Dysphagia![]() , an impairment in swallowing solid foods and liquids, is also present in Huntington's Disease. Dysarthria and dysphagia developing and worsening during the disease can lead to respiratory problems, which is why pneumonia is a common cause of death in people with HD.
, an impairment in swallowing solid foods and liquids, is also present in Huntington's Disease. Dysarthria and dysphagia developing and worsening during the disease can lead to respiratory problems, which is why pneumonia is a common cause of death in people with HD.
Parkinson's syndrome![]() is a set of symptoms characteristic of Parkinson's Disease, which can occur not only in the course of this disease but also with other conditions. Parkinsonian symptoms also occur in Huntington's Disease and may influence misdiagnosis. This group of symptoms progresses over time. It includes, but is not limited to, the bradykinesia mentioned earlier.
is a set of symptoms characteristic of Parkinson's Disease, which can occur not only in the course of this disease but also with other conditions. Parkinsonian symptoms also occur in Huntington's Disease and may influence misdiagnosis. This group of symptoms progresses over time. It includes, but is not limited to, the bradykinesia mentioned earlier.
Other symptoms of parkinsonism include postural rigidity and instability. These usually lead to falls and injuries in the advanced stages of the disease. Parkinsonism is often observed with little or no symptoms of chorea. This type of disease is common in seniors with late detection of HD.

The majority of patients with HD have cognitive impairment. Cognitive abilities include sensory processes or sense perception. Cognitive skills also include attention and memory. In addition, reasoning and logical thinking. Cognitive deficits in Huntington's Disease can precede motor symptoms for many years. In HD patients, these processes can be impaired to varying degrees. Mental symptoms, therefore, include:
Patients in the early stages of the disease may experience limitations in various executive functions, including difficulties in decision-making. Some people are inherently more indecisive than others. This type of difficulty may be influenced by other factors such as stress, anxiety, and low self-esteem. However, in Huntington's disease, the cause is neurodegeneration, causing cognitive impairment.
Cognitive disorders can also present as difficulties in organization and planning. Organizational skills include completing assigned tasks, estimating how long it will take to complete them, and planning tasks well into the future. Therefore, patients with Huntington's Disease cognitive disorders may have problems with everyday activities such as planning shopping and remembering necessary appointments and chores.
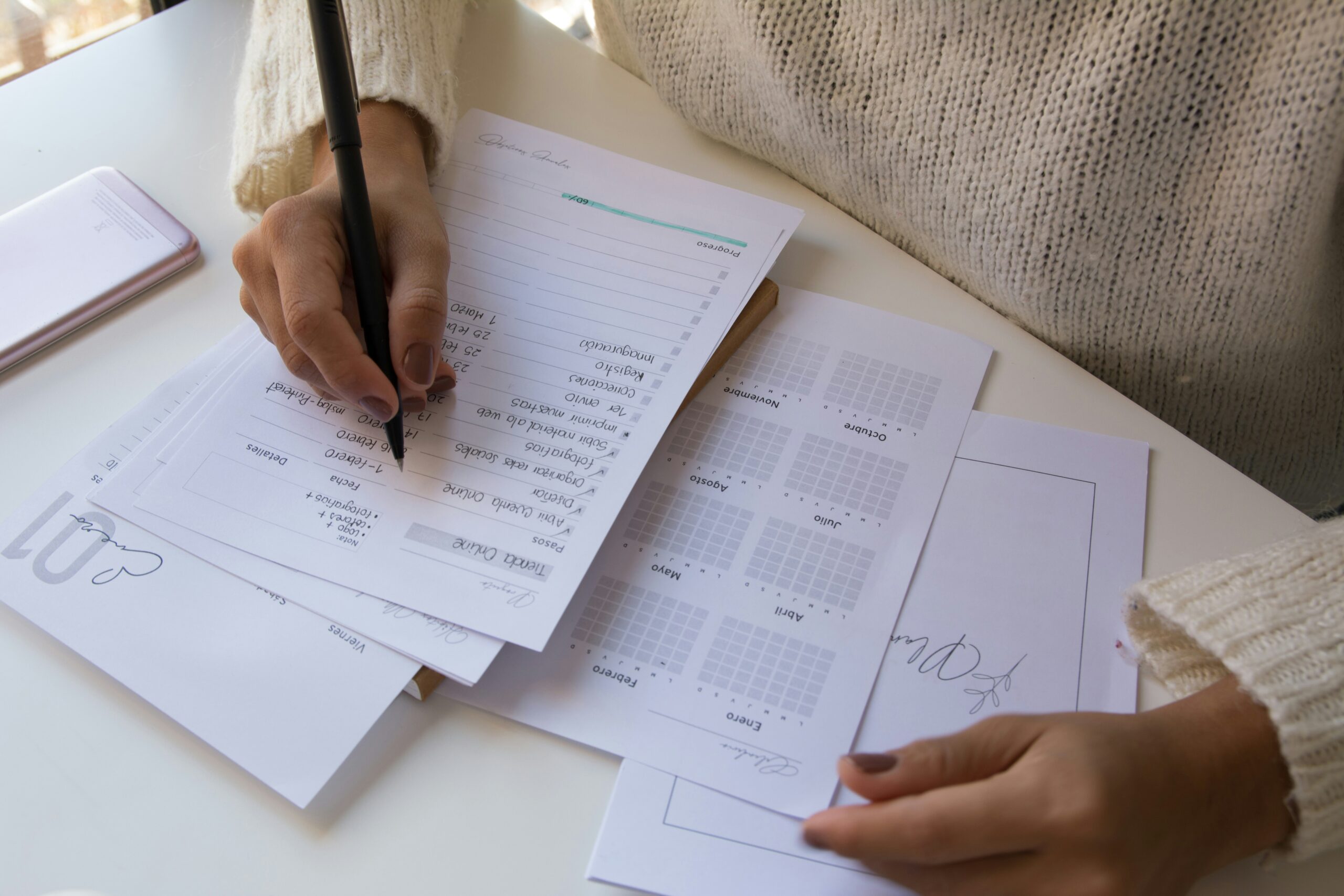
Multitasking is the ability to perform several activities at the same time and perform them at an appropriate level. People who do not have a neurological disorder may also have difficulties multitasking. However, for people with HD, cognitive impairment significantly limits the performance of tasks and responsibilities, especially over time as the disease progresses.
Dementia is a medical condition in which intellectual function is progressively impaired. A person with dementia develops memory problems and slowed thinking. As the cognitive symptoms of HD worsen, dementia states of increasing severity occur. Dementia in Huntington's disease is subcortical![]() , meaning that memory loss is due to ineffective memory retrieval. In the dementia of HD patients, features such as apraxia and aphasia are absent, as they are in dementia syndrome only. In addition, psychomotor processes are significantly slowed down.
, meaning that memory loss is due to ineffective memory retrieval. In the dementia of HD patients, features such as apraxia and aphasia are absent, as they are in dementia syndrome only. In addition, psychomotor processes are significantly slowed down.
Psychiatric symptoms of Huntington's disease can be varied, and the range is wide. Most commonly, psychiatric symptoms are associated with frontal lobe dysfunction, which is consistent with the pathophysiology of the disease. Again, the intensity of these symptoms varies as the disease progresses. Initially, they may be mild personality changes leading to psychiatric disorders that require care and treatment. Psychiatric symptoms include:

At the onset of the disease, the first warning sign for close Huntington's Disease patients is their personality change. Patients suddenly or gradually begin to behave differently than before. This is particularly true of people who were previously calm and non-confrontational and who, as the disease progresses, begin to express aggression![]() . The lack of emotional regulation increases distress in family and friends of Huntington's disease patients.
. The lack of emotional regulation increases distress in family and friends of Huntington's disease patients.
As the disease progresses, Huntington's Disease patients become increasingly unable to control their emotions. Initially, there is minor irritability and impulsivity; over time, this increases to outbursts of anger and aggression. In addition to irritability or anger, mood swings include sudden onset of sadness, inner tension, bursts of crying alternating with cheerfulness, and feelings of inner peace.
Apathy, a state of indifference and loss of interest in everyday life, may occur in the later stages of the illness. This is accompanied by a lack of energy and motivation, a lack of life goals, a decreased sensitivity to emotional stimuli, and less interaction with other people. Patients lose creativity and curiosity and do not take initiative. The patients' families often then suspect the presence of depression, but emotional blandness in HD is not always associated with feelings of sadness, hopelessness, and bad mood. Apathy is a prevalent feature of Huntington's disease.

Depression is expected in the course of Huntington's Disease. However, it is not known whether depressive states are related to the neurodegeneration process. Depression usually occurs in the early stages of HD. Regarding depression, there is also a risk of suicide![]() in patients who are most severely depressed at the time of diagnosis. Therefore, it is presumed that depressive states are not related to the disease process but rather to the patient's psychological response to the disease.
in patients who are most severely depressed at the time of diagnosis. Therefore, it is presumed that depressive states are not related to the disease process but rather to the patient's psychological response to the disease.
Psychiatric symptoms also include increased anxiety, psychotic symptoms, delusions, and hallucinations. Psychotic disorders manifest themselves in consciousness, thinking, perception, and behavior. The sufferer cannot perceive their thinking and perceptions as illogical and inconsistent with reality. In addition, cases of obsessive-compulsive disorder![]() are also possible. However, these types of disorders are much less frequent than, for example, depressive disorders.
are also possible. However, these types of disorders are much less frequent than, for example, depressive disorders.
The diagnosis of Huntington's chorea should begin with a history, during which the doctor will highlight psychiatric, cognitive, and motor dysfunctions. In addition to this, it is also essential to carry out appropriate examinations, which include:

Genetic testing is highly effective in diagnosing HD. It detects changes in DNA![]() and provides important information about a person's health. Genetic tests are increasingly available and of growing importance in modern medical care. The result of a genetic test confirms the presence of a mutation in the Huntington's gene, which ultimately confirms the disease. Genetic testing can also be performed in at-risk individuals with a family history of the disease.
and provides important information about a person's health. Genetic tests are increasingly available and of growing importance in modern medical care. The result of a genetic test confirms the presence of a mutation in the Huntington's gene, which ultimately confirms the disease. Genetic testing can also be performed in at-risk individuals with a family history of the disease.
Before genetic testing is carried out, basic tests can be performed. Many data necessary for diagnosing HD can also be extracted from lab tests. This is particularly important when distinguishing the disease from other similar syndromes. Therefore, creatine kinase and liver enzyme levels are tested to be able to distinguish HD from McLeod syndrome![]() .
.
MRI is also used to diagnose Huntington's Disease. The results show brain volume and brain connections. this way, neurodegenerative changes can be seen, even several years before the onset of symptoms. Later in the disease process, cerebellar atrophy is observed. MRI can also distinguish HD from other diseases, such as cerebellar ataxia.
There is no cure for Huntington's disease. The treatment of HD is based on therapeutic options for improving quality of life through the reduction of symptoms. There are various treatment methods, which include:
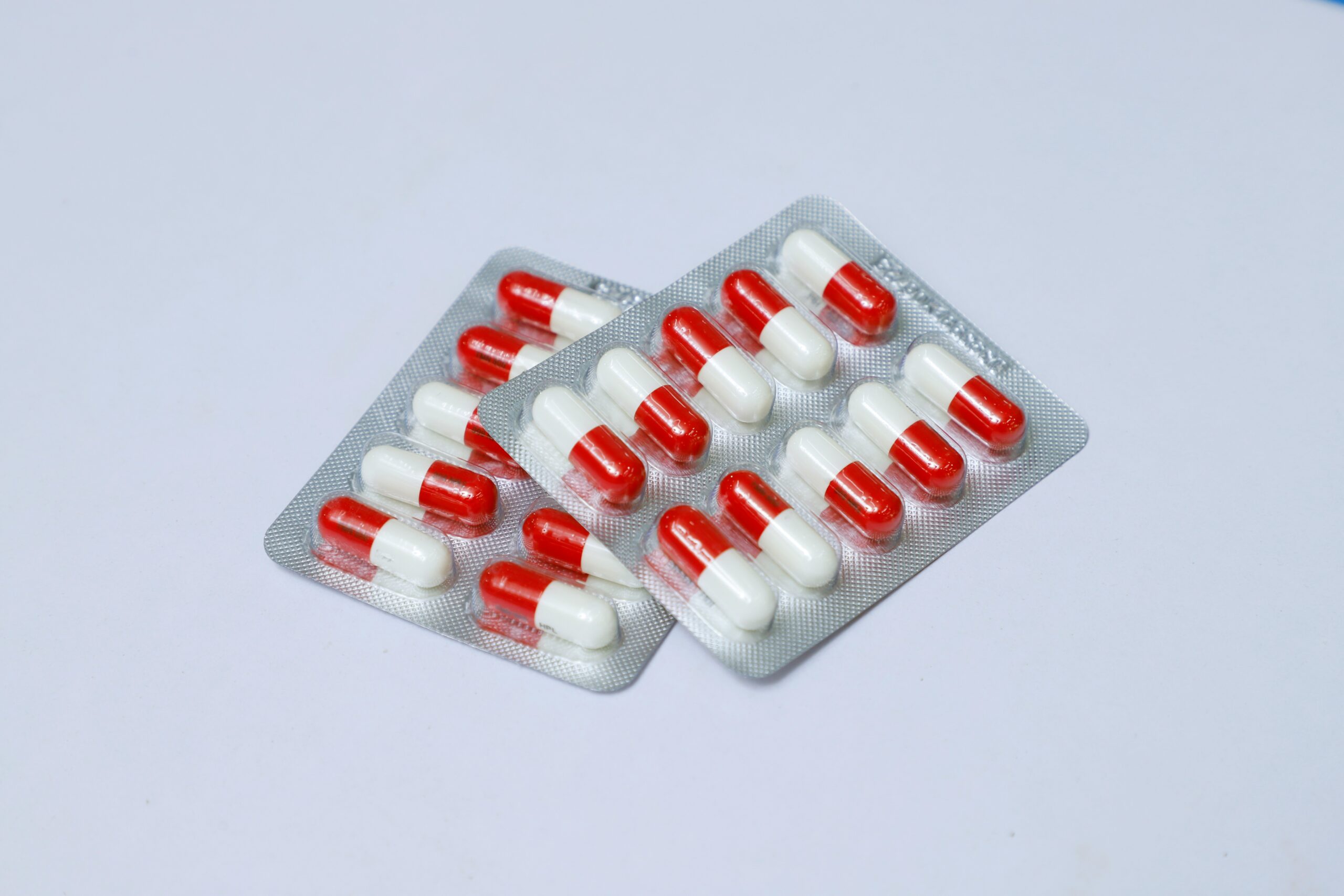
Treatment of HD is mainly pharmacological and supportive. According to the American Academy of Neurology![]() , drugs such as tetrabenazine, a********e, or r******e are used in the treatment of chorea. However, these drugs can cause potential side effects. These include depression, which can be exacerbated. Other commonly used drugs include dopamine antagonists, which are considered in the treatment of chorea and psychosis. Antiparkinsonian drugs such as l******a may be regarded as in some patients. Antidepressants are also used in HD to treat depression, anxiety, and obsessive-compulsive disorder.
, drugs such as tetrabenazine, a********e, or r******e are used in the treatment of chorea. However, these drugs can cause potential side effects. These include depression, which can be exacerbated. Other commonly used drugs include dopamine antagonists, which are considered in the treatment of chorea and psychosis. Antiparkinsonian drugs such as l******a may be regarded as in some patients. Antidepressants are also used in HD to treat depression, anxiety, and obsessive-compulsive disorder.
Surgical treatment is possible but does not play an essential role in Huntington's Disease. Several surgical options have been evaluated for their effectiveness in suppressing chorea. Deep brain stimulation![]() is a neurosurgical operation to improve patients' quality of life. This treatment method will not cure the disease, but it significantly reduces the symptoms of HD. DBS involves the implantation of thin stimulating electrodes into deeply located parts of the brain. The implanted electrodes generate electrical impulses that affect the activity of the nerve centers that cause the disease.
is a neurosurgical operation to improve patients' quality of life. This treatment method will not cure the disease, but it significantly reduces the symptoms of HD. DBS involves the implantation of thin stimulating electrodes into deeply located parts of the brain. The implanted electrodes generate electrical impulses that affect the activity of the nerve centers that cause the disease.
A new therapeutic approach for treating HD is gene therapy, which offers promising advances in its prevention![]() . Gene therapy involves silencing the mutated genes responsible for the disease. Therefore, gene therapy has a neuroprotective effect without disease symptoms. However, these are only predictions that may be confirmed in future studies.
. Gene therapy involves silencing the mutated genes responsible for the disease. Therefore, gene therapy has a neuroprotective effect without disease symptoms. However, these are only predictions that may be confirmed in future studies.
Non-pharmacological treatment, including environmental changes and therapy should also be considered where possible. Due to the risk of psychological distress, patients with Huntington's Disease receive psychological care. These include behavioral or cognitive therapies that have a supportive effect on the patient's mental state. This is particularly important, especially if the patient has severe depression or other disorders. Patients with HD are at risk of suicide. All patients should be monitored for symptoms of depression as well as suicidal thoughts.
In addition to psychological care, patients with HD need ongoing general care, especially in the late stages of the disease. As HD progresses, patients have limited functioning and should have caregivers to help them move around and carry out daily activities. Special attention is also paid to diet. Unhealthy lifestyles, smoking, and alcohol consumption are discouraged. Families caring for HD patients can rely on particular support associations.

Huntington's disease is an incurable and progressive neurodegenerative disease. The duration of HD is usually 15 to 20 years![]() . Depending on the course of the disease, the duration can vary. The progression of Huntington's disease leads to total dependence on daily life. Patients must be thoroughly cared for until the end of their lives.
. Depending on the course of the disease, the duration can vary. The progression of Huntington's disease leads to total dependence on daily life. Patients must be thoroughly cared for until the end of their lives.
The most common cause of death in people with Huntington's Disease is pneumonia![]() , in which breathing difficulties occur. Another common cause is suicide
, in which breathing difficulties occur. Another common cause is suicide![]() . Unfortunately, there are also no methods to prevent Huntington's disease. Genetic counseling can play an important role, which is helpful for people diagnosed with the disease and their families. Such action aims to increase awareness of those at risk of developing the disease, possibly contributing to earlier diagnosis.
. Unfortunately, there are also no methods to prevent Huntington's disease. Genetic counseling can play an important role, which is helpful for people diagnosed with the disease and their families. Such action aims to increase awareness of those at risk of developing the disease, possibly contributing to earlier diagnosis.
Huntington's chorea is a genetically determined disease of the central nervous system. The causes lie in genetics, and the disease is inherited in an autosomal dominant manner. The occurrence of the disease depends on mutations in the HTT gene. Symptoms of the disease appear in patients between 30 and 50 years of age, but cases before 20 are also possible. Huntington's disease mainly manifests itself with motor, cognitive, and psychiatric disorders. Usually, the onset of Huntington's chorea is hardly noticeable, and symptoms worsen over time.
The course of the disease can vary from individual to individual. The most characteristic is the motor symptoms, which initially present as clumsiness and, over time, take the form of rapid, uncontrolled movements. The diagnosis of Huntington's chorea should begin with a history, during which the doctor will highlight psychiatric, cognitive, and motor dysfunctions. Various medical tests such as laboratory, imaging, or genetic tests are also used. A complete cure for HD is impossible, but therapeutic options exist to improve patients' lives.