Apraxia is a disorder that means the inability to perform precise, complex, and purposeful movements. A person struggling with this problem fully understands the activity but cannot conduct it. At the same time, they do not have any paresis, motor coordination disorders, sensory disorders, muscle weakness, or cerebellar symptoms that would prevent them from undertaking a given activity.
The term “apraxia” was proposed in 1908 by Hugo Liepmann, a German doctor specializing in neurology and psychiatry. The researcher also observed that the critical structure for the praxis system (the ability to perform purposeful movements) is the left cerebral hemisphere.
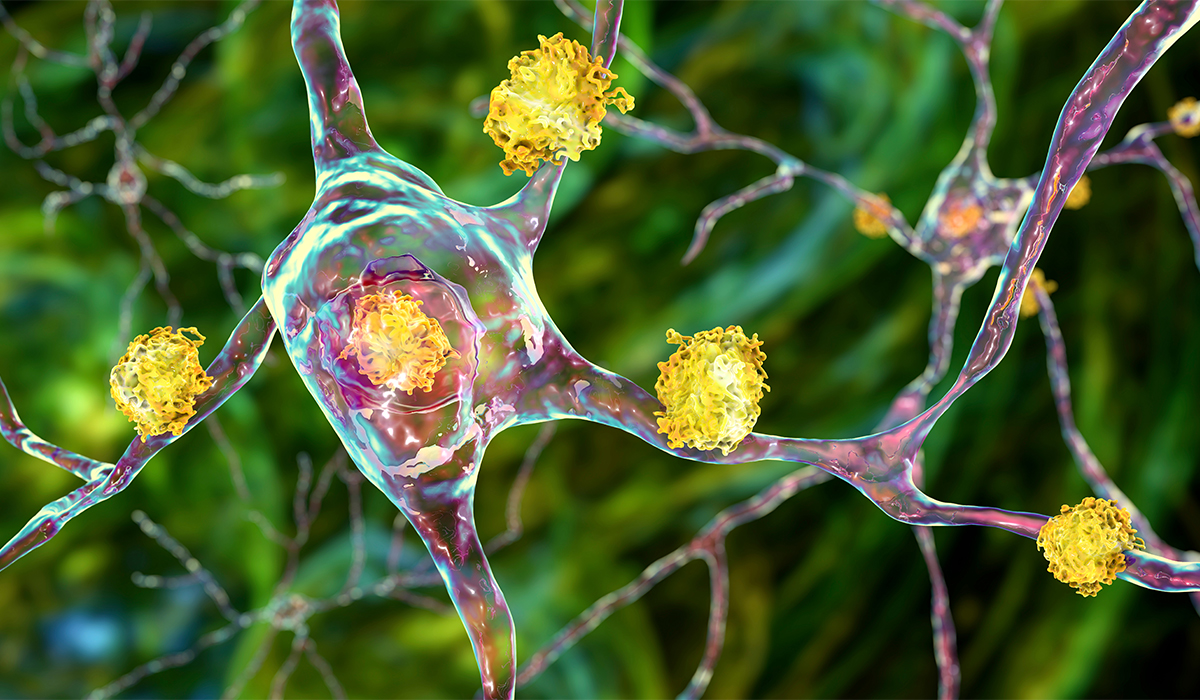
The cause of apraxia![]() is direct damage to the cerebral cortex in the areas that remember complex motor activities and are responsible for their implementation. It means that the symptoms are not related to abnormalities in the musculoskeletal system. Apraxia may appear, among others, after strokes, brain tumors, brain injuries, and brain inflammation, as well as in the course of neurodegenerative diseases (e.g., Parkinson's disease). In children, apraxia may also be congenital.
is direct damage to the cerebral cortex in the areas that remember complex motor activities and are responsible for their implementation. It means that the symptoms are not related to abnormalities in the musculoskeletal system. Apraxia may appear, among others, after strokes, brain tumors, brain injuries, and brain inflammation, as well as in the course of neurodegenerative diseases (e.g., Parkinson's disease). In children, apraxia may also be congenital.

Neurology distinguishes several types of apraxia![]() . The specialists based this division on the location of damaged brain centers and the resulting clinical picture of a given type of apraxia.
. The specialists based this division on the location of damaged brain centers and the resulting clinical picture of a given type of apraxia.
Limb-kinetic apraxia![]() results from damage to the back part of the frontal lobe, the so-called premotor area. It causes clumsiness in motor activities performed in the opposite half of the body. It means that motor apraxia of the limbs on the right side of the body will be a consequence of a defect located in the left cerebral hemisphere. A patient with motor apraxia can plan a complex motor act, but their movements are uncertain, e.g., they give the impression of instability while walking.
results from damage to the back part of the frontal lobe, the so-called premotor area. It causes clumsiness in motor activities performed in the opposite half of the body. It means that motor apraxia of the limbs on the right side of the body will be a consequence of a defect located in the left cerebral hemisphere. A patient with motor apraxia can plan a complex motor act, but their movements are uncertain, e.g., they give the impression of instability while walking.
Limb-kinetic apraxia is a specific type of kinetic motor apraxia, but in its case, the problem affects the entire body, not individual limbs or muscle groups.
Ideomotor skills involve the ability to repeat intentional or purposeless gestures of other people and to follow commands. The specialists sometimes call this type of condition mixed apraxia because during it the patient knows and remembers the plan of complex movements sequences but is only can perform simple, long-learned activities.
Ideomotor disorders include buccofacial apraxia![]() , which happens when attempting to pantomime actions or mouth movements imitating words spoken by the examiner.
, which happens when attempting to pantomime actions or mouth movements imitating words spoken by the examiner.
Ideomotor apraxia![]() results from damage to the parietal lobe of the dominant hemisphere. Due to this location, it is often accompanied by other neurological deficit symptoms, most often aphasia, i.e., loss of the ability to speak, and agnosia, i.e., the inability to recognize sensory stimuli while maintaining the functions of the sense organs.
results from damage to the parietal lobe of the dominant hemisphere. Due to this location, it is often accompanied by other neurological deficit symptoms, most often aphasia, i.e., loss of the ability to speak, and agnosia, i.e., the inability to recognize sensory stimuli while maintaining the functions of the sense organs.
Constructional apraxia![]() is a spatial-visual disorder. It manifests itself in the loss of the ability to draw simple objects (e.g., a house) and construct (e.g., using blocks). Constructional apraxia determines the inability to perform movements in a falsely perceived space.
is a spatial-visual disorder. It manifests itself in the loss of the ability to draw simple objects (e.g., a house) and construct (e.g., using blocks). Constructional apraxia determines the inability to perform movements in a falsely perceived space.
Ideational apraxia![]() accompanies diffuse disease processes of the cerebral cortex (apraxia in Alzheimer's disease, apraxia in cerebral arteries, apraxia after stroke). Its essence is a chaotic confusion of simple motor components, which causes the patient to behave like an indecisive, disorderly person,
accompanies diffuse disease processes of the cerebral cortex (apraxia in Alzheimer's disease, apraxia in cerebral arteries, apraxia after stroke). Its essence is a chaotic confusion of simple motor components, which causes the patient to behave like an indecisive, disorderly person,
Oculomotor apraxia![]() involves the absence or profound impairment of controlled, purposeful eye movements. People with this type of apraxia have trouble with horizontal, rapid eye movements and tracking other repositioning objects. Ocular apraxia is usually associated with congenital deficiencies of the central nervous system and is a common subtype of apraxia in children.
involves the absence or profound impairment of controlled, purposeful eye movements. People with this type of apraxia have trouble with horizontal, rapid eye movements and tracking other repositioning objects. Ocular apraxia is usually associated with congenital deficiencies of the central nervous system and is a common subtype of apraxia in children.
Apraxia of speech![]() , like visual apraxia, is often diagnosed in childhood when the child begins to say their first words. The causes of apraxia of speech are still unclear. Its undoubted distinguishing feature is the lack of initiation and coordination of jaw, lip, and tongue movements. A child with apraxia of speech requires intensive speech therapy as soon as possible.
, like visual apraxia, is often diagnosed in childhood when the child begins to say their first words. The causes of apraxia of speech are still unclear. Its undoubted distinguishing feature is the lack of initiation and coordination of jaw, lip, and tongue movements. A child with apraxia of speech requires intensive speech therapy as soon as possible.

This problem is classified as a linguistic deficit. It is characterized by abnormalities at the stage of planning, controlling, or programming the movements necessary for speaking, i.e., within the articulators. It means that the sick person knows what they want to say but cannot translate it into articulatory movements.
It is worth realizing that apraxia of speech rarely occurs on its own. Most often, it coexists with aphasia or dysarthria. Additionally, there may be other deficits related to damage to the left brain hemisphere, including spasticity or apraxia of the limbs (these affect the right side of the body). Therefore, a sick person may have problems not only communicating verbally but also using gestures.
A separate disorder is nonverbal oral apraxia![]() . We talk about it when a person cannot perform movements of the facial muscles and articulatory organs (e.g., rounding the lips). However, apraxia of speech has a much broader context.
. We talk about it when a person cannot perform movements of the facial muscles and articulatory organs (e.g., rounding the lips). However, apraxia of speech has a much broader context.
Apraxia of speech in children is a congenital neurological disorder. It is probably related to the lack of innate ability to create articulatory movements that correspond to given sounds. It may be related to the immaturity of brain structures. It happens that childhood apraxia of speech occurs with other disorders – e.g., autism spectrum disorder.
AOS occurs regardless of disorders of language functions such as understanding, reading, writing, and naming. Unlike aphasia![]() , which takes the form of multimodal linguistic deficits, as an isolated condition it only affects verbal expression. Of course, it can and often does coexist with aphasia.
, which takes the form of multimodal linguistic deficits, as an isolated condition it only affects verbal expression. Of course, it can and often does coexist with aphasia.
Therefore, clinically we may be dealing with a primary form of AOS, i.e., with a deficit revealed as a result of a specific etiology, or with a secondary form, which is a descending form of the disorder after the resolution of aphasia with which it coexisted primarily, which often leads to diagnostic errors consisting in classifying her to dysarthria (due to the lack of reading, writing, understanding and naming disorders). Both may also coexist permanently.
The similarity of aphasia and AOS may result in the latter being classified as limb-kinetic or conduction aphasia. The systematic co-occurrence of both conditions and the rarity of pure AOS make the differential diagnosis very challenging. It is also not made easier by the neuroanatomical features (frontal and left-sided temporoparietal regions from the left middle artery vascularization) and etiological aspects (predominance of strokes), which are not significantly diverse.
Also, the types of errors that appear are not the pure form of AOS more often occur in connection with damage to the posterior part of the frontal lobe or insula than to temporoparietal lesions, while aphasia without AOS more often occurs as a result of deficits in the temporal or temporoparietal areas.
In the case of aphasia, errors are most likely linguistic or phonological (they take the form of phonemic paraphasias), while in AOS they result from motor planning or programming disorders, and therefore their specificity is phonetic, as they take the form of substitution, accretion, transposition, elision, in other words, phonetic paraphasia.
According to specialists, errors in conductive aphasia include a deficiency in the selection of phonemes, and individuals with AOS can make this selection but have issues with it. The difference between them is that in conduction aphasia the prosody is close to normal, while in AOS there are numerous pauses, speech is strained and therefore far from correct prosody. It does not change that both conditions are comparable in the sound level of errors made. The articulation of a patient with AOS is very disturbed, as well as the prosody and pace of speech. Syllables are clearly distinguished, and the spaces between words increase.
For comparison, in fluent aphasia, e.g., sensory aphasia, speech rate, and prosody are normal. In the speech of people with AOS, substitutions, and deformations are noticeable and articulated with effort and hesitation. In aphasic utterances, even those made with hesitation and effort, there are no deformations and there are phonemes specific to a given language.
According to researchers, practical errors are closer to articulatory patterns than phonological errors in people with aphasia without apraxia of speech. Also, repeated repetition in AOS results in less variation in the structure of the resulting words compared to aphasic trials. Basically, in distinguishing between aphasia and AOS, it is essential to consider language functions other than motor ones because, in isolated apraxia of speech, there are no impairments in understanding, reading, writing, or naming. Thus, the comparison of the quality of spoken and written language is valuable in the differential diagnosis of AOS and aphasia.
As shown above, apraxia of speech is often associated with aphasia. Dysarthria![]() , on the other hand, rarely co-occurs with aphasia. It does not change the fact that dysarthria may coexist with apraxia of speech.
, on the other hand, rarely co-occurs with aphasia. It does not change the fact that dysarthria may coexist with apraxia of speech.
The resemblance between AOS and dysarthria is connected to the fact that individuals with apraxia of speech also have the liability of the facial and tongue muscles on the right side. Both conditions have a similar etiology, AOS often appears as a result of hemorrhagic strokes, which are also the cause of dysarthria. The latter also appears in neurodegenerative diseases, as well as AOS. Dysarthrias occur more often in the case of subcortical than cortical lesions, while AOS most likely occurs more often as a result of cortical lesions.
Unlike dysarthria, AOS is not associated with impaired functioning of articulatory muscles. The patient does not present any paralysis or paresis and does not have any problems with non-linguistic skills such as chewing, swallowing, or coughing. Disturbed speech cannot be explained by the possible presence of weakness of the tongue or face muscles; it is inappropriate to the degree of reduced muscle tone and weakened articulator motor skills. Therefore, in the case of speech apraxia, utterances (during repetition) are disturbed inconsistently, periodically they may be closer to the articulatory pattern of the word being searched for or even coincide with it but after a while, they become very disturbed.
The motor deficit results from disturbed planning or programming, not the executive capabilities of the muscular apparatus. Automatic speech is slightly more efficient in apraxia of speech. The quality of statements is influenced by the factors of frequency of occurrence, word length, and semantic content. However, dysarthric speech is uniformly impaired, the patient produces utterances to the best of their current articulatory capabilities, e.g., with paresis of the tongue, palate, or lips. People with AOS try to correct their statements before they start to implement them statement, they try to look for the correct pattern, which is not something that patients with dysarthria do.
They also differ to some extent in the types of mistakes they make. In dysarthria, simplifications or deformations of speech sounds are observed. In the case of AOS, we are talking not only about deformations, but also about substitutions, growth, repetition, and extension, which brings the mentioned errors closer to aphasic realizations. Errors in AOS are very diverse, irregular, and unpredictable, visible, especially in unlearned, previously unrealized utterances. This phenomenon is rather the instability in the implementation of given articulatory systems.
Dyspraxia![]() is difficulty in performing sequential tasks and problems with coordination, processing stimuli, and remembering, which affects the body's nervous and immune systems. Dysfunctions in the fields of motor coordination disorders, motor learning, and perception disorders are also characteristic features of the described problem.
is difficulty in performing sequential tasks and problems with coordination, processing stimuli, and remembering, which affects the body's nervous and immune systems. Dysfunctions in the fields of motor coordination disorders, motor learning, and perception disorders are also characteristic features of the described problem.
Very often, dyspraxia is called the clumsy child syndrome. The most classic example of this type of abnormality in a child is the inability to sequence complex motor tasks. It may be, for example, a problem with completing individual stages when brushing your teeth.

Verbal dyspraxia means articulatory and phonatory dysfunctions. The child often speaks too quietly and misses certain sounds, sometimes even entire areas of speech, which may make them incomprehensible and illogical. There are often problems with proper breathing and sensation in the mouth.
Motor dyspraxia is a dysfunction most often manifested by difficulty in performing tasks consisting of several sequences. The motor coordination of such a child is well below the age norm and his intellectual capabilities. The dysfunction is observed at a very early stage of development and is not the result of neurological disorders or diseases. It is not acquired. It causes difficulties in activities, e.g., learning steps during dance rehearsals, preparing a meal, dressing, and washing.
Unfortunately, the term dyspraxia has different meanings depending on who uses it. Some people use the word dyspraxia interchangeably with apraxia. Others use the term developmental dyspraxia to describe certain disorders in children and apraxia in adults. According to some specialists, apraxia is the loss of abilities that one has, and dyspraxia is a dysfunction in the development of these abilities. They use the term developmental dyspraxia to emphasize that it is a disorder in the development of certain abilities and not the result of damage to the CNS.
Treatment for apraxia![]() depends primarily on the underlying cause. After consulting a doctor, it is assessed whether a given case requires surgical or pharmacological treatment. Some types of apraxia may prove incurable and rehabilitation is necessary.
depends primarily on the underlying cause. After consulting a doctor, it is assessed whether a given case requires surgical or pharmacological treatment. Some types of apraxia may prove incurable and rehabilitation is necessary.
The prognosis depends on certain factors – primarily the severity and type of the disease that resulted in the symptoms of apraxia. Unfortunately, this disease is often progressive. Therefore, in most cases, the prognosis is not favorable.
Table of Contents
Dyspraxia is a perceptual and motor dysfunction manifested by developmental coordination disorders. How does it manifest itself? What is the… read more »
Aphasia is the loss of language abilities in various areas – understanding speech, pronouncing logical sentences, naming objects. What are… read more »
Huntington's disease is genetically determined. No effective cure has yet been developed, but research into modern treatments is ongoing. Learn… read more »

The nervous system is divided into many parts, and each part has specific functions. Learn about the function and diseases… read more »

Ataxia is a motor coordination issue when individuals struggle with exact movements, holding the correct posture, or having standard walking… read more »

Angelman syndrome is a neurogenetic disorder that is often misdiagnosed. Find out what the characteristic symptoms are and learn about… read more »
ASMR is the feeling of a pleasant tingling in the body, created in response to external sensory stimuli. What triggers… read more »

Vascular dementia can occur after a stroke or other incident. Learn the most important information to recognize early symptoms and… read more »

Tourette syndrome is characterized by tics. What are its causes? What to do if we observe disturbing symptoms? read more »