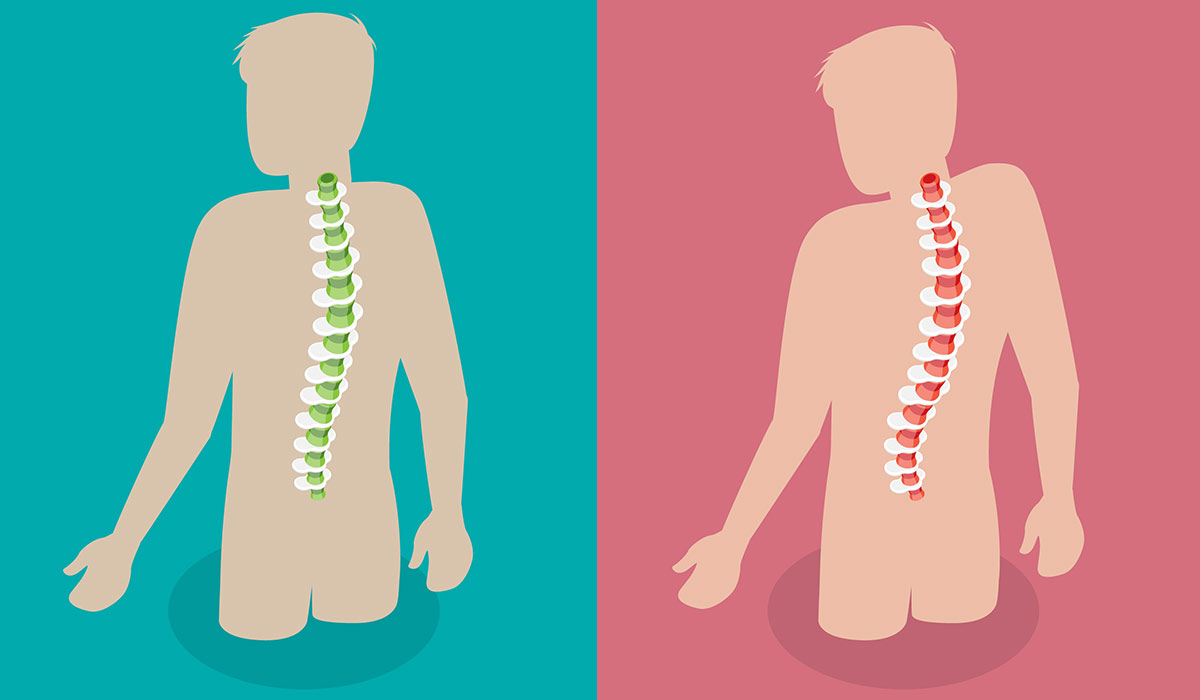
Ankylosing spondylitis (AS) is a chronic inflammatory disease that attacks the spine, causing it to be painful and stiff. Its intensity varies – from mild to very severe. In the advanced form of the disease, bone fusions are formed at the flexible connections of the vertebrae, causing progressive limitation of spine mobility.
The result is a forward tilt of the body (so-called kyphosis) and severe disability. The disease may also affect other joints (e.g., hip, shoulder) and diverse organs (e.g., eyes, heart, and lungs). A characteristic feature of AS is inflammation of the sacroiliac joints, connecting the base of the spine with the pelvis.
The actual cause![]() of ankylosing spondylitis
of ankylosing spondylitis![]() is unspecified. Probably, for the disease to develop, several factors must combine: genetic, immunological (immune system disorders), and environmental, such as bacterial infections (especially the gastrointestinal and urogenital tracts).
is unspecified. Probably, for the disease to develop, several factors must combine: genetic, immunological (immune system disorders), and environmental, such as bacterial infections (especially the gastrointestinal and urogenital tracts).
Genetic factors play a significant role, which is confirmed by the fact that the risk of developing the disease is higher if a close relative suffers from AS. In many white patients, the so-called HLA B27 antigen![]() is a genetic marker of this disease.
is a genetic marker of this disease.
The onset and course of ankylosing spondylitis may vary between patients. Atypical symptoms![]() occur more often in women, so the disease is diagnosed later.
occur more often in women, so the disease is diagnosed later.
Low back pain![]() is usually the first to appear, radiating to the buttocks (on one or both sides, often alternating). The pain is dull, difficult to localize, and gradually increases over several weeks or months. It has the nature of inflammatory pain, which has several characteristic features:
is usually the first to appear, radiating to the buttocks (on one or both sides, often alternating). The pain is dull, difficult to localize, and gradually increases over several weeks or months. It has the nature of inflammatory pain, which has several characteristic features:

In some cases (especially in women), cervical spine pain may appear first. In the early stages of the disease, low-grade fever/fever, loss of appetite, feeling of general disarray, and fatigue may also occur.
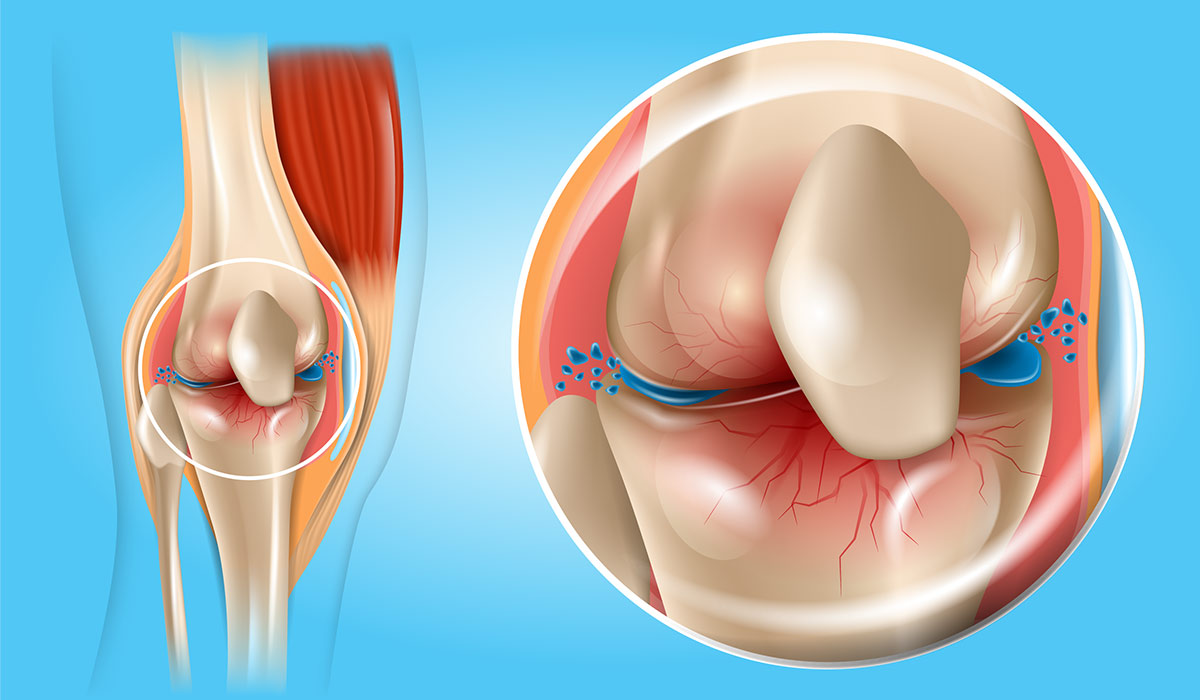
In a few patients, the first symptom of ankylosing spondylitis is pain in locations other than the spine, caused by inflammation of other joints (e.g., hip, ankle, or knee) or inflammation of the so-called tendon insertions, i.e., places where a tendon or ligament connects with a bone (e.g., heel pain due to inflammation of the Achilles tendon insertion). In some cases, the onset of musculoskeletal symptoms precedes uveitis or enteritis for several years.
As the disease progresses, pain, stiffness, and limited mobility also affect the higher spine levels.
Involvement of the cervical spine causes, among others, trouble turning your head back, which makes driving difficult. Changes in the thoracic spine and ribs reduce the expansion of the chest when taking in air (that's why patients breathe mainly through the diaphragm). Chest pain and tenderness may appear, intensifying with deep inhalation, coughing, and sneezing – they are most often caused by inflammation of the joints of the chest but require differentiation from other diseases, e.g., lung and heart diseases.
Limited spine mobility makes it difficult to perform various daily activities, e.g.:
The disease is often accompanied by fatigue, which is the result of, among others, chronic inflammation and sleep problems.
The spine of a patient with AS is more sensitive to injuries, which results from the loss of elasticity and the faster development of osteoporosis in this disease. It can lead to instability and subluxation of the spine or vertebral fractures, even after a minor injury, e.g., after falling from a height. It may damage the spinal cord and the nerves coming from it.
In the advanced form of the disease, which is fortunately becoming less common, there is a complete loss of spine mobility and severe disability![]() . The patient has a characteristic, forward-leaning figure, which makes it difficult for them to look forward and move. Deformation and contracture of other joints (especially hip and knee joints) often occur.
. The patient has a characteristic, forward-leaning figure, which makes it difficult for them to look forward and move. Deformation and contracture of other joints (especially hip and knee joints) often occur.
In addition to the symptoms listed above, pain, swelling, and limited mobility of other joints![]() may also occur, e.g., hips, knees, ankle joints, shoulders, connections of the ribs with the spine and sternum, jaw joints, as well as small joints of the hands and feet. These are the so-called peripheral symptoms of AS.
may also occur, e.g., hips, knees, ankle joints, shoulders, connections of the ribs with the spine and sternum, jaw joints, as well as small joints of the hands and feet. These are the so-called peripheral symptoms of AS.
Some patients with AS suffer from one or more episodes of inflammation of part of the eye (the so-called uvea![]() ). Symptoms usually occur on one side; these are:
). Symptoms usually occur on one side; these are:
They require urgent consultation with an ophthalmologist – if left untreated they may lead to vision loss. In some patients, uveitis may occur before other disease symptoms appear.
In the course of AS, atherosclerosis![]() and its complications develop more quickly, e.g., ischemic heart disease. It is the result of activation of inflammatory processes. In addition, there may be:
and its complications develop more quickly, e.g., ischemic heart disease. It is the result of activation of inflammatory processes. In addition, there may be:
Many patients with AS have decreased chest expansion![]() during inspiration due to stiffening of the connections between the ribs and the spine, but this rarely causes breathing disorders because patients reflexively breathe through the diaphragm. Breathing problems and lung damage occur much more often in patients who smoke cigarettes – pulmonary fibrosis and severe respiratory infections may occur.
during inspiration due to stiffening of the connections between the ribs and the spine, but this rarely causes breathing disorders because patients reflexively breathe through the diaphragm. Breathing problems and lung damage occur much more often in patients who smoke cigarettes – pulmonary fibrosis and severe respiratory infections may occur.
In ankylosing spondylitis, endoscopic examinations of the gastrointestinal tract![]() very often reveal non-specific inflammatory changes in the intestines (probably involved in this disease development), which usually do not cause any clinical symptoms. Some patients suffer from ulcerative colitis or Crohn's disease. Gastric and duodenal ulcers are also more common in the course of AS, which is facilitated by the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to control pain and stiffness.
very often reveal non-specific inflammatory changes in the intestines (probably involved in this disease development), which usually do not cause any clinical symptoms. Some patients suffer from ulcerative colitis or Crohn's disease. Gastric and duodenal ulcers are also more common in the course of AS, which is facilitated by the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to control pain and stiffness.
The spine's role includes, among others protecting the spinal cord and the nerves coming from it. Damage to nervous structures may occur in the event of vertebral subluxation or fracture, which in patients with AS may occur even after a minor injury or fall.
Some neurological symptoms![]() include:
include:
If you experience symptoms of ankylosing spondylitis, do not delay in seeking medical attention. Low back pain is typical and often goes away on its own, but a quick consultation with a rheumatologist requires the so-called inflammatory pain. Brief diagnosis and treatment of the disease significantly increase the chance of avoiding its complications, including severe disability.
Exacerbation of the symptoms of the disease also requires an immediate visit to a rheumatologist. Treatment must then be intensified to deal with the pain and inflammation as quickly as possible. Severe pain causes the body to reflexively assume incorrect positions (“contract into itself”), increasing stiffening of the spine and leading to joint contractures. Try to maintain correct body posture and return to daily exercise as soon as possible, avoiding excessive strain on the joints. In addition to medications (NSAIDs, painkillers), applying ice bags to painful areas (10-15 minutes, 3-4 times a day) or taking a warm bath or shower may help combat pain.
During ankylosing spondylitis, situations may occur that require urgent consultation with a doctor.
Eye pain and redness, light sensitivity, and vision problems indicate uveitis, requiring prompt treatment by an ophthalmologist.
Any neurological symptoms – numbness, tingling, decreased sensation, muscle weakness or paresis of limbs, problems with controlling urination and defecation, a significant increase in neck pain – may indicate damage to neural structures and in some cases require urgent surgical intervention.
Chest pain, shortness of breath, and decreased exercise tolerance may indicate heart or lung disease and require urgent diagnosis.
Planned pregnancy (applies to both women and men) – AS is not a contraindication to pregnancy and does not affect its course. However, it should be planned to discontinue some medications that may harm the fetus early enough.
A doctor (usually a rheumatologist) diagnoses AS![]() based on information obtained from the patient, examination of the musculoskeletal system, and the results of imaging and laboratory tests. When examining the patient, the doctor assesses the mobility of the spine in all directions (e.g., when leaning forward, bending to the side, turning the head back, expanding the chest when breathing deeply) and examines whether there is pain and tenderness in places characteristics of AS, such as sacroiliac joints, spine, around the attachment of the ribs to the sternum and spine, and the heels.
based on information obtained from the patient, examination of the musculoskeletal system, and the results of imaging and laboratory tests. When examining the patient, the doctor assesses the mobility of the spine in all directions (e.g., when leaning forward, bending to the side, turning the head back, expanding the chest when breathing deeply) and examines whether there is pain and tenderness in places characteristics of AS, such as sacroiliac joints, spine, around the attachment of the ribs to the sternum and spine, and the heels.

Each patient with suspected AS should undergo an X-ray of the sacroiliac joints to look for signs of inflammation, e.g., bone erosions. Unfortunately, these changes are usually visible only after several years of the disease. In doubtful cases, when symptoms of the disease occur and no typical changes are detected on X-ray, nuclear magnetic resonance imaging (MRI) is helpful, thanks to which inflammatory changes can be detected much faster. To assess the spine, X-rays are taken, and sometimes also computed tomography (CT) or magnetic resonance imaging (MRI) (e.g., when pressure on neural structures is suspected). In case of symptoms of arthritis and enthesitis, an ultrasound examination (USG) is helpful.
In addition to imaging tests, laboratory tests are also performed.
HLA-B27![]() is a protein – human leukocyte antigen B27 (HLA-B27) – found on the surface of white blood cells. The presence of the HLA-B27 antigen is associated with an increased risk of some autoimmune diseases. An autoimmune condition happens when the immune system attacks its cells.
is a protein – human leukocyte antigen B27 (HLA-B27) – found on the surface of white blood cells. The presence of the HLA-B27 antigen is associated with an increased risk of some autoimmune diseases. An autoimmune condition happens when the immune system attacks its cells.
Thanks to them, the immune system identifies its cells, distinguishing them from foreign ones. HLA antigens are characterized by the fact that they are inherited and the combination is present on the surface of specific cells and white blood cells. The composition of HLA antigens is necessary in the case of transplantation treatment because there must be compatibility of HLA combinations in the donor and recipient.
The sensitivity of the HLA-B27 test is so high that the marker is used not only to confirm the diagnosis in people with advanced changes. Diagnostic importance also gains in the early stage of the disease, when the symptoms do not indicate its development. HLA-B27 as a genetic marker works very well in assessing the likelihood of developing ankylosing spondylitis. Based on the obtained result, it is possible to determine the intensification of the disease process in the future, identifying patients at a very high risk of a severe course.
The test result does not determine the diagnosis or exclusion of the disease. It is used as one of the tests in the diagnostic process of specific autoimmune diseases and should be interpreted together with clinical symptoms and other laboratory and imaging tests to confirm or exclude the diagnosis.
Treatment with NSAIDs![]() slows down the progression of the disease and inhibits the calcification of the paraspinal ligaments. Corticosteroids
slows down the progression of the disease and inhibits the calcification of the paraspinal ligaments. Corticosteroids![]() are also used in AS.
are also used in AS.
When the painkillers used prove to be unreliable, in some cases the treatment includes a drug from the group of TNF-alfa inhibitors![]() (anti-tumor necrosis factor), which is administered in the form of injections. It helps reduce inflammation and slow down the development of the disease.
(anti-tumor necrosis factor), which is administered in the form of injections. It helps reduce inflammation and slow down the development of the disease.
Sometimes, an advanced form of AS leads to significant damage to the joints and spine. In rare cases, surgery![]() is performed to improve the spinal axis and surgically correct deformities. Surgical treatment in the case of hip joint involvement also involves replacing the diseased joint with a prosthesis.
is performed to improve the spinal axis and surgically correct deformities. Surgical treatment in the case of hip joint involvement also involves replacing the diseased joint with a prosthesis.
Pharmacological treatment is supported by correctly conducted physiotherapy![]() , which includes not only breathing and physical exercises but also hydrotherapy and massages to relax the body. Exercise should be used in all patients.
, which includes not only breathing and physical exercises but also hydrotherapy and massages to relax the body. Exercise should be used in all patients.
For a healthy life with AS, it is necessary to avoid:

Curing the disease is currently not possible![]() . In isolated cases, the disease resolves spontaneously. However, we have medications that effectively control symptoms and improve the patient's functioning. Some of them, such as NSAIDs and biologics, may also inhibit the progression of the disease.
. In isolated cases, the disease resolves spontaneously. However, we have medications that effectively control symptoms and improve the patient's functioning. Some of them, such as NSAIDs and biologics, may also inhibit the progression of the disease.
Ankylosing spondylitis can occur in many different ways. Currently, thanks to appropriate treatment, in most circumstances we are dealing with a mild form of the disease, which only slightly impairs normal functioning. The first ten years of the disease are particularly significant for further prognosis – this is when functional impairment, changes in peripheral joints, and radiological changes in the spine most often occur. That is why it is so important to quickly diagnose and actively fight the disease from the very beginning. However, in some patients, AS has a severe course, leading to significant disability and shortened life expectancy.
Because ankylosing spondylitis is a chronic disease, regular rheumatological follow-up is necessary. The frequency of visits depends on the disease activity and the treatment used. Appropriate questionnaires, the progress of changes during the examination of the musculoskeletal system, and the results of imaging and laboratory tests are used to assess the severity of the disease.
Control X-rays of the spine are performed no more often than every two years (unless there is suspicion of rapid progression of the disease or other changes, e.g., vertebral fracture). As a rule, there is no point in repeating the X-ray of the sacroiliac joints if they have already shown changes typical of AS. However, follow-up X-rays of the hip joints (their involvement indicates a more severe course of the disease) or the cervical spine (risk of changes in the vertebrae causing neurological changes) are helpful.
Table of Contents
Spondylosis is a degenerative change in the spine that usually occurs with age. Find out how to recognize the disease… read more »

A rheumatologist is a doctor who specializes in rheumatic diseases, which are diseases of joints, muscles, and bones. What tests… read more »

Muscle pain and stiffness – these can be the first symptoms of arthritis. Learn about the most common types of… read more »
Scoliosis is a structural deformation of the spine that occurs in three planes. What are its causes and symptoms? What… read more »

Back pain is among the most common causes of productivity loss in the US. What causes it? How do you… read more »

Sciatica is a set of symptoms resulting from irritation or damage to the sciatic nerve or its roots. How is… read more »

Psoriatic arthritis is a long-lasting inflammatory disease of the joints in patients with psoriasis, which can cause joint destruction and… read more »

Ehlers-Danlos Syndrome is a group of diseases with a genetic basis. Learn all the symptoms associated with EDS. Find out… read more »
Osteoarthritis is a disease that most often affects children and the elderly. What are its causes? How can it be… read more »