Vascular Dementia is a dementia in which brain damage of vascular origin is considered the cause of the disease. It is a heterogeneous group of disorders and can result from various vascular abnormalities, both ischemic and posthemorrhagic lesions.
Vascular-derived dementias can also be divided into different types, determined by the location and size of the lesions.
Vascular dementia is irreversible, progressive, and challenging to treat. However, unlike neurodegenerative conditions such as Alzheimer's, the onset of vascular dementia can be actively prevented by influencing its etiological factors, including controlling blood pressure and lipid metabolism.
Causes of vascular dementia include:
Vascular dementia primarily develops from a singular incident, like a stroke![]() or intracranial hemorrhage, that causes vascular damage and brain hypoxia. Occasionally, it can arise due to prolonged processes within the central nervous system. In this context, the so-called small vessel disease of the brain, caused by hypertension and gene mutations, is particularly mentioned.
or intracranial hemorrhage, that causes vascular damage and brain hypoxia. Occasionally, it can arise due to prolonged processes within the central nervous system. In this context, the so-called small vessel disease of the brain, caused by hypertension and gene mutations, is particularly mentioned.
Vascular dementia is the result of ischemic damage to brain tissue. Ischemia, or hypoperfusion, can be caused by vascular disease of large and small caliber or develop against a background of intracerebral hemorrhages. In this case, the following two types of vascular dementia are distinguished:
Multi-infarct dementia![]() is caused by widespread, multiple cortical-subcortical infarcts or strategic strokes of tiny but critical cognitive function brain regions. Multi-infarct dementia develops due to extensive vessel disease, usually after a strategic, cortical, subcortical, or cerebral hemorrhage.
is caused by widespread, multiple cortical-subcortical infarcts or strategic strokes of tiny but critical cognitive function brain regions. Multi-infarct dementia develops due to extensive vessel disease, usually after a strategic, cortical, subcortical, or cerebral hemorrhage.
Post-stroke dementia results from the closure of the arterial lumen and, thus, restriction of blood supply to the brain. Subsequent stages of ischemic necrosis of nerve cells are associated with massive atherosclerotic lesions in the large intracerebral arteries or with displacement of embolic material, often originating from cardiac cavities.
Hemorrhagic episodes, or rapid extravasation of blood directly into the brain tissue, on the other hand, are favored by blood clotting disorders, aneurysms and microaneurysms, and congenital vascular malformations.
Pathology of multiple smaller cerebral vessels, which results, among other things, from untreated hypertension, is responsible for most cases of progressive vascular dementia. Vascular dementia associated with stenosis and decreased blood flow in small vessels includes Binswanger's disease![]() and small vessel disease
and small vessel disease![]() .
.
Binswanger's disease: Binswanger's disease is caused by years of poorly controlled hypertension leading to leukoencephalopathy, or diffuse damage to the subcortical white matter, with fibrosis of the small vessels and sometimes necrosis of the large arteries that feed brain tissue.
Small vessel disease: The second type of dementia associated with small-vessel disease, on the other hand, arises due to impairment of the brain tissue surrounding the finest infiltrating arterioles. Such lacunar stroke foci may remain asymptomatic for a long time.
Patients with vascular dementia can have different symptoms depending on the cause and the brain area affected. The general and most common symptoms of vascular dementia include:
Personality Disorders – In individuals with vascular dementia, a notable observation is the abrupt alteration in their personality traits![]() . Gradually, patients exhibit behaviors distinct from their previous demeanor, which close friends and family members may pick up on. Among the common indications are tendencies to act out of line or respond inappropriately to circumstances. Additionally, heightened levels of anxiety or aggression may manifest where they hadn't before in affected patients.
. Gradually, patients exhibit behaviors distinct from their previous demeanor, which close friends and family members may pick up on. Among the common indications are tendencies to act out of line or respond inappropriately to circumstances. Additionally, heightened levels of anxiety or aggression may manifest where they hadn't before in affected patients.
Lack of Control – Patients with vascular dementia experience a loss of control, particularly in performing certain activities. They struggle to adapt their behavior to the situation, face difficulties maintaining attention, and encounter problems with orientation. In addition, loss of control may manifest as sphincter dysfunction, including urinary and fecal incontinence. These challenges stem from brain damage and result in a patient losing command over various essential functions.
Mood Changes – Mood changes can often be observed as a prevalent symptom of vascular dementia. Patients frequently experience heightened irritability and have a tendency to display emotional outbursts. Additionally, they may endure periods of depression![]() and lose interest in their once beloved passions. Though less common, some individuals may also withdraw from daily activities, during the advanced stages of dementia, apathy, indifference, and occasional aggression become more dominant.
and lose interest in their once beloved passions. Though less common, some individuals may also withdraw from daily activities, during the advanced stages of dementia, apathy, indifference, and occasional aggression become more dominant.
Memory Deterioration – Memory deterioration is a common symptom in various forms of dementia. However, it does not always manifest in cases of vascular dementia. In vascular dementia, memory decline occurs when the stroke or hemorrhage damages the memory centers. The loss or decay of brain cells can lead to impaired memory function. However, in subcortical leukoencephalopathy, memory impairment![]() , and higher cortical functions are rare.
, and higher cortical functions are rare.
Cognitive Impairment – Cognitive abilities![]() are the skills used to perform various actions and activities. Patients with vascular dementia may, therefore, experience problems with planning and carrying out planned activities. Weakening intellectual abilities can result in difficulties concentrating and acquiring new knowledge. Additionally, cognitive processes may slow down progressively over time. Individuals facing such challenges may require assistance in decision-making and may experience issues with orientation.
are the skills used to perform various actions and activities. Patients with vascular dementia may, therefore, experience problems with planning and carrying out planned activities. Weakening intellectual abilities can result in difficulties concentrating and acquiring new knowledge. Additionally, cognitive processes may slow down progressively over time. Individuals facing such challenges may require assistance in decision-making and may experience issues with orientation.
Movement Disorders – Symptoms of vascular dementia often encompass movement disorders, including difficulties with balance maintenance. This condition may lead to gait and balance disorders, increasing the risk of falls and impeding independent movement. As the disease progresses, individuals may face challenges in performing basic daily activities such as dressing themselves and necessitating constant care.
Neurological Deficits – Vascular dementia can result in neurological deficits like paresis![]() or aphasia. These deficits occur when the nervous system in the motor pathway, responsible for transmitting nerve impulses from the cerebral cortex to muscles, gets damaged—paresis refers to limited range of motion or decreased muscle strength. Conversely, aphasia signifies a loss of language ability across different areas. It is caused by damage to the brain, specifically its left hemisphere, due to a stroke. Weakness of one side of the body or one-sided paralysis can also occur due to brain lesions.
or aphasia. These deficits occur when the nervous system in the motor pathway, responsible for transmitting nerve impulses from the cerebral cortex to muscles, gets damaged—paresis refers to limited range of motion or decreased muscle strength. Conversely, aphasia signifies a loss of language ability across different areas. It is caused by damage to the brain, specifically its left hemisphere, due to a stroke. Weakness of one side of the body or one-sided paralysis can also occur due to brain lesions.
Vascular dementia is a condition that can have two different developmental paths. Its course can be sudden and rapid or slow and gradual.
When vascular dementia follows a stroke or other individual event, symptoms appear suddenly and in large numbers. They are very pronounced from the beginning, and in the later stages, they deepen by leaps and bounds, unlike Alzheimer's disease, which develops gradually, even imperceptibly at first.
In contrast, when dementia occurs as a result of small vessel disease, the process is staggered. It usually begins with subtle symptoms, and then gradually, more symptoms appear, increasing their intensity.
If vascular dementia is slow and gradual, the stages of the disease can be noted. The intensity and number of symptoms change over time in such a course.
At the beginning of the disease, symptoms can be challenging to recognize. The first impairments of various brain functions appear, depending on the case. Minor mobility or the first memory problems may make remembering difficult. The first mood and personality changes also occur at this stage. Patients, however, can control most of the functions that keep them functional and independent in their activities.
In the more advanced stage of the disease, individuals experience severe cognitive impairments and a limited understanding of their condition. At this point, simple tasks like using household appliances and phones become challenging, necessitating increased attention and support—additionally, memory and speech difficulties become more pronounced. While patients still retain some independence, continuous care is essential.
In severe dementia, there is a complete breakdown of personality. Patients may not recognize objects or people close to them. They have difficulty with essential functions such as eating and following hygiene rules. They are constrained and may be completely unable to speak or move. The extent of symptoms depends on the case; however, at this stage, patients require constant support from a caregiver.
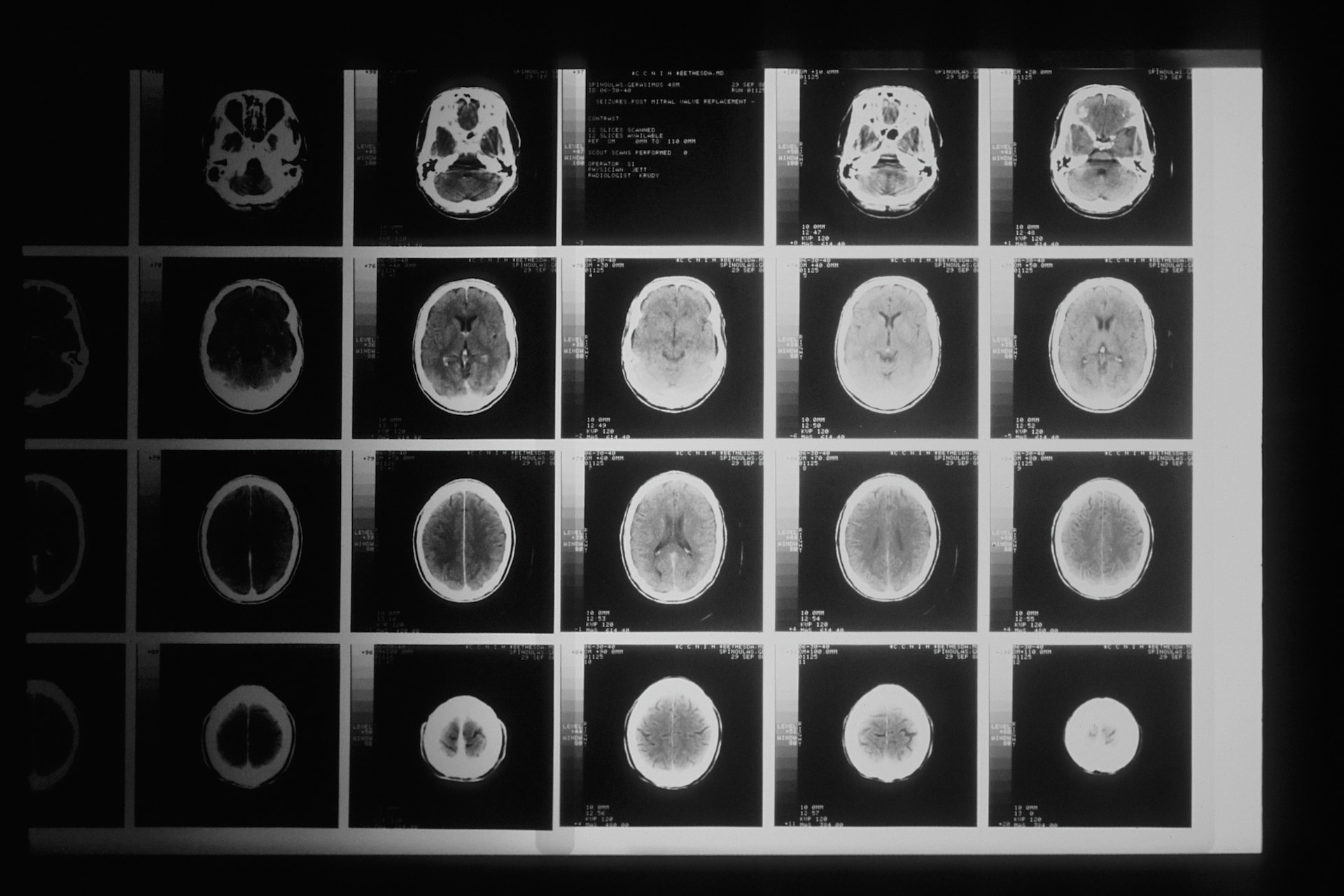
To diagnose vascular dementia syndrome, it is necessary to establish a causal relationship between typical dementing symptoms and a vascular episode or a history of generalized vascular disease. Dementia can be diagnosed only 6 months after the onset of symptoms impairing daily functioning while excluding the presence of disturbances of consciousness. The following tools and tests are used to diagnose vascular dementia:
Written tests, like the Mini-Mental State Examination![]() and the Clock Test
and the Clock Test![]() , are crucial in diagnosing cognitive impairment. The MMSE test comprises 30 questions designed to assess cognitive dysfunction. Conversely, the Clock Test is a widely used screening tool for detecting dementia and mild cognitive impairment. It provides an indicative rating of mental disability when suspecting dementia, especially in its early stages.
, are crucial in diagnosing cognitive impairment. The MMSE test comprises 30 questions designed to assess cognitive dysfunction. Conversely, the Clock Test is a widely used screening tool for detecting dementia and mild cognitive impairment. It provides an indicative rating of mental disability when suspecting dementia, especially in its early stages.
Additionally, imaging tests such as MRI and CT scans aid in identifying cerebrovascular diseases by revealing stroke foci. In cases where vascular dementia is suspected, these tests help identify cortical and subcortical atrophy, focal vascular lesions, and areas affected by ischemic strokes. Laboratory tests are also valuable for ruling out reversible causes of dementia.
The choice of treatment usually depends on the cause. Most often, drug treatment and prophylaxis are used.
Unfortunately, all the changes that have occurred are irreversible. With the help of treatment, it is only possible to slow the further course of the disease. In this case, various types of drugs are used, which are determined by the doctor. Often, symptomatic medications are also implemented, depending on what symptoms appear in the patient. These may include preparations for insomnia or to combat anxiety.
Prevention should also be taken care of in patients with dementia. Primary prevention of vascular brain damage should be based on permanent lifestyle changes: diet and physical activity to maintain a normal BMI, stop smoking, and reduce alcohol consumption.
It is now believed that the most critical factors that increase the likelihood of vascular dementia are uncontrolled hypertension and lipid disorders. Blood pressure-lowering drugs and pharmacological therapy for diabetes and hypercholesterolemia significantly reduce the risk of secondary cerebral vascular diseases.
Vascular brain damage is permanent, so a complete cure is impossible. The prognosis for vascular dementia is not as good as in all other cases of dementia. Due to the irreversible nature of the lesions, it is only possible to alleviate the symptoms or slow the further progression of the disease, but there is no cure.
Therefore, one should be aware that the therapy undertaken will not produce spectacular results; moreover, the first immediate results may not be noticeable until many months have passed. The essential point of therapeutic management remains inhibiting disease progression with appropriate pharmacotherapy of dementing symptoms and diseases predisposing to central nervous system ischemia.
Some people may be at risk for vascular dementia. In such cases, prevention is recommended to reduce the risk of developing the disease in later years. Risk factors for vascular dementia are:

Diabetes – Type 2 diabetes is a decisive factor in cognitive impairment in seniors. This is especially true for those patients with poor glycemic control. The association between diabetes and dementia may be driven by several mechanisms. One potential mechanism involves peripheral metabolic disorders![]() that indirectly harm the brain.
that indirectly harm the brain.
Obesity – Obesity has been extensively researched, revealing a confirmed connection between obesity![]() and dementia. Studies indicate that individuals who are obese have a significantly higher likelihood of developing dementia compared to those within a healthy weight range. Moreover, obese individuals with other metabolic disorders may experience a faster decline in mental performance.
and dementia. Studies indicate that individuals who are obese have a significantly higher likelihood of developing dementia compared to those within a healthy weight range. Moreover, obese individuals with other metabolic disorders may experience a faster decline in mental performance.
Hypertension – An analysis of studies reveals that hypertension![]() , or high blood pressure, negatively impacts the brain's blood vessels. This interference results in damage to the white matter, an integral component for cognitive function. Consequently, the risk of dementia may significantly increase.
, or high blood pressure, negatively impacts the brain's blood vessels. This interference results in damage to the white matter, an integral component for cognitive function. Consequently, the risk of dementia may significantly increase.
Cardiac Arrhythmias – In particular, a condition such as atrial fibrillation is the most common type, associated with an increased possibility of some forms of dementia. Heart disorders![]() can lead to heart attack or stroke, which raises the risk of vascular dementia.
can lead to heart attack or stroke, which raises the risk of vascular dementia.
Strokes – A stroke occurs when a part of the brain dies due to disrupted blood flow. Having experienced previous strokes![]() can heighten the risk of developing vascular dementia. Additionally, stroke serves as a decisive contributing factor that significantly raises the chances of developing dementia.
can heighten the risk of developing vascular dementia. Additionally, stroke serves as a decisive contributing factor that significantly raises the chances of developing dementia.
Generalized Arteriosclerosis – Generalized arteriosclerosis![]() occurs when lipid plaques build up on the artery walls, gradually narrowing blood flow. If an atherosclerotic plaque or thrombus breaks away, it can lead to cerebral ischemia and an ischemic stroke. These conditions often result in paralysis, hemiparesis, aphasia, and in severe cases, even death.
occurs when lipid plaques build up on the artery walls, gradually narrowing blood flow. If an atherosclerotic plaque or thrombus breaks away, it can lead to cerebral ischemia and an ischemic stroke. These conditions often result in paralysis, hemiparesis, aphasia, and in severe cases, even death.
Cigarette Smoking – The link between cigarette smoking and the development of neurodegenerative diseases is attributed to the inflammation caused by smoking![]() . The toxins present in cigarettes can harm blood vessels, leading to blockage of blood flow or inadequate supply to the brain. Consequently, brain cells may perish due to this reduced blood circulation.
. The toxins present in cigarettes can harm blood vessels, leading to blockage of blood flow or inadequate supply to the brain. Consequently, brain cells may perish due to this reduced blood circulation.
Alcohol Abuse – Excessive consumption of alcohol![]() has been associated with the development of various conditions, including dementia. Alcohol can contribute to the development of condition like dementia by affecting brain structure and function. Excessive alcohol consumption is related to a greater risk of early-onset dementia.
has been associated with the development of various conditions, including dementia. Alcohol can contribute to the development of condition like dementia by affecting brain structure and function. Excessive alcohol consumption is related to a greater risk of early-onset dementia.
Age Over 65 – Dementia most often affects older people, but cases of dementia among younger people have also been reported in medicine as a result of genetic and biological factors.
There are numerous types of dementia, each with its course of progression. It is estimated that there are over 100 different types of dementia, and the specific symptoms experienced largely depend on the underlying cause of the disease. So by reason, the most common types of dementia can be distinguished:
This is the most common type of dementia. Its development may go unnoticed for a long time, explained by absentmindedness or old age. The first signs of Alzheimer's disease may seem subtle, such as occasional forgetfulness of new information. However, these initial symptoms generally do not disrupt the patient's daily life significantly. As the condition progresses, difficulties arise in assimilating and retaining any fresh information.
Alzheimer's disease typically manifests initially through short-term memory loss, challenges with word retrieval, and alterations in personality and mood. With further advancement of the disease, long-term memory gradually declines along with abilities like reading comprehension, logical reasoning, and effective communication with others.
The development of Alzheimer's stems from brain shrinkage caused by amyloid deposits and neurofibrillary clusters that impede efficient information transmission between cells, ultimately leading to cellular death![]() . The brain ceases to function efficiently, so the patient has increasing problems with memory and speaking, walking, and performing daily activities.
. The brain ceases to function efficiently, so the patient has increasing problems with memory and speaking, walking, and performing daily activities.
Usually, the causes of dementia are mainly neurodegenerative diseases, Whereas vascular dementia is caused by damage to blood vessels in the brain![]() . The brain does not get as much blood with oxygen and nutrients as it needs. A stroke or intracranial hemorrhage causes brain damage of vascular origin. Hypertension can also have a crucial effect on the development of vascular dementia.
. The brain does not get as much blood with oxygen and nutrients as it needs. A stroke or intracranial hemorrhage causes brain damage of vascular origin. Hypertension can also have a crucial effect on the development of vascular dementia.
This disorder, which causes a general decline in cognitive functioning, is characterized by impairment of such functions as memory, attention, thinking, and orientation. Dementia usually develops in stages. This means that all symptoms appear gradually.
Exceptions are emergencies, such as a stroke or intracranial hemorrhage. In such a situation, symptoms may appear suddenly and in large numbers. Vascular dementia can resemble Alzheimer's disease. Moreover, it is not uncommon for the two conditions to co-occur.
Dementia with Lewy bodies is a type of dementia caused by the presence of Lewy bodies in the brain. These structures contribute to the deterioration of the dopamine-producing center![]() . Consequently, individuals diagnosed with this form of dementia often experience challenges such as attention deficit disorders, difficulties with logical thinking, and problems related to movement.
. Consequently, individuals diagnosed with this form of dementia often experience challenges such as attention deficit disorders, difficulties with logical thinking, and problems related to movement.
This is a neurodegenerative disease in which pathological changes occur in the central nervous system. Dementia with Lewy bodies is difficult to recognize condition. It can be misdiagnosed by some as Alzheimer's or Parkinson's disease. Proper diagnosis is critical.
Typical symptoms are hand tremors. If the earthquakes occur when the patient tries to reach for something or do something, it may be a symptom of dementia with Lewy bodies. For dementia with Lewy bodies, mental symptoms – visual hallucinations, delusions, depression – are most characteristic.
Frontotemporal dementia results from degeneration in the brain's frontal and temporal lobes![]() . Depending on which brain area is damaged, the disease will be accompanied by different symptoms. The main diagnostic point of frontotemporal dementia is a head imaging study highlighting atrophic changes in specific areas.
. Depending on which brain area is damaged, the disease will be accompanied by different symptoms. The main diagnostic point of frontotemporal dementia is a head imaging study highlighting atrophic changes in specific areas.
Frontal lobe dementia is primarily manifested by changes in behavior, mainly increased aggression. Temporal lobe disease, on the other hand, manifests as problems with communication and understanding messages. The lesions most often appear in people aged 50-60, but frontal-temporal dementia is also seen in younger people.
In the course of typical frontotemporal dementia, patients develop behavioral and mental disorders. These consist, for example, of neglect of personal hygiene, excessive psychomotor activity, and loss of the ability to maintain interpersonal contacts.
Sometimes, different types of dementia can occur at the same time. For example, it is possible to have vascular dementia and Alzheimer's disease together, at the same time. Mixed dementia occurs as a result of two or more simultaneously developing pathological processes.
The incidence of mixed dementia remains uncertain. In recent years, there has been an increase in the diagnosis of mixed dementia; however, this may be attributed to challenges in identifying its symptoms. It is particularly noteworthy that seniors are more likely to experiencing multiple types of dementia.
Vascular dementia often occurs due to a stroke or other violent events, leading to memory lapses and difficulty performing daily activities. This condition is characterized by progressive impairment of cognitive functions and emotions that interfere with daily functioning.
The symptoms depend on the location of vascular diseases and damage to the brain. Vascular dementia can manifest in different ways: sudden and unexpected symptoms may arise with blood clots or strokes, while symptoms develop gradually with repeated occurrences over time.
Diagnosis involves assessing mental state and cognitive function and conducting neuroimaging studies. Unfortunately, vascular dementia is incurable; however, drug treatment aims to delay its progression and provide symptomatic relief. It typically manifests around age 65, sharing essential risk factors with stroke episodes.