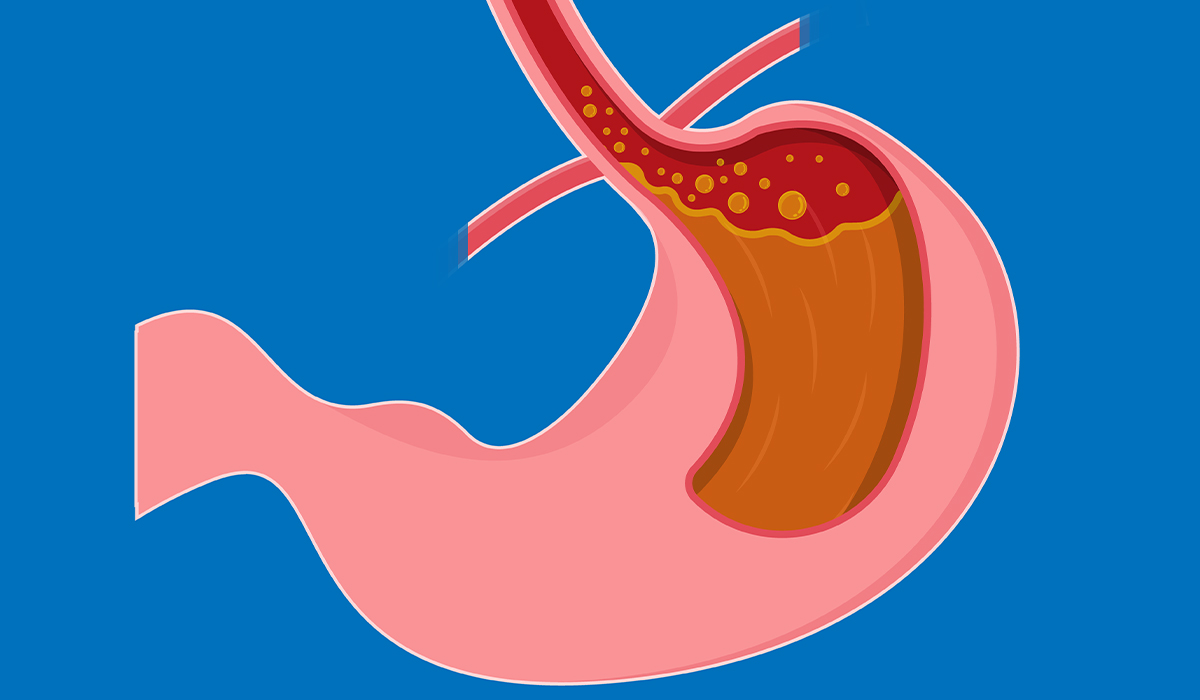
Gastroparesis is a disorder of upper gastrointestinal motility. Gastroparesis means paralysis of the stomach. It consists of a cessation of gastric emptying without a demonstrable mechanical cause.
Gastroparesis is a chronic condition, the essence of which is delayed emptying of the stomach, which significantly affects patients' quality of life. The disease causes a backlog of food content in the stomach, stretching its walls.
Gastroparesis can have a variety of causes. One of the most commonly cited is diabetes. In addition tothis, different diseases and conditions can contribute to gastritis. It is often impossible or complicated to pinpoint the cause. Gastroparesis is a whole set of clinical symptoms associated with impaired stomach motility. Patients in advanced stages of gastroparesis may experience dehydration and malnutrition.

The symptoms of gastroparesis are so non-specific that the disease is difficult to diagnose. Similar symptoms are found in many different conditions. The diagnosis of gastroparesis is based on the demonstration of delayed gastric emptying in a patient with typical symptoms while excluding mechanical obstruction. In diagnosing the condition, tests are done to assess the stomach's motility. The pharmacological treatment of gastroparesis is based on the use of prokinetic drugs. In addition, diet is of great importance. Untreated gastroparesis can cause various complications, which can harm the patient's health.
In the general population, gastroparesis is most often idiopathic. It means that in nearly half of the patients, no apparent cause for the condition can be determined. During infection, the postulated mechanism is damage to autonomic neurons of the stomach wall or gastric pacemaker cells.
The normal motor function of the stomach includes the active relaxation of the smooth muscles of the proximal part of the stomach after a meal and the peristaltic contractions that are good for the maximum fragmentation of the food content. This is followed by gradually emptying small portions of finely ground food. Stretching of the stomach by food activates reflexes from the vagus nerve, which causes an active reduction in the tension of the stomach wall muscles. The stomach's motor activity is regulated at many levels; it is a complex mechanism. It involves the central nervous system, autonomic system, neurotransmitters, and, locally, the stomach wall cells.

Gastroparesis is a disorder of peristaltic movements of the gastrointestinal tract, which is a consequence of nerve damage, which in turn causes disorders of the stomach musculature. Neurological changes![]() contribute to gastroparesis. As a result of this disease, there is a slowdown or even stasis in the process of moving food content from the stomach to the duodenum. The stomach walls become disturbed, which can lead to the formation of undesirable structures made up of undigested debris. Since it is accompanied by increased fermentation of food, bacteria also appear. Gastroparesis can be a consequence of many diseases.
contribute to gastroparesis. As a result of this disease, there is a slowdown or even stasis in the process of moving food content from the stomach to the duodenum. The stomach walls become disturbed, which can lead to the formation of undesirable structures made up of undigested debris. Since it is accompanied by increased fermentation of food, bacteria also appear. Gastroparesis can be a consequence of many diseases.
Causes that can cause the described pathomechanism include:
Gastroparesis is a risk in people with diabetes. Among the more severe types of this condition is diabetic gastroparesis, which is a consequence of diabetic complications![]() . Studies show that hyperglycemia contributes to the slowing down of stomach emptying processes in both healthy and diabetic people. Hyperglycemia states are associated with reduced frequency of contractions of the stomach fundus, slowing of peristaltic action, development of abnormal rhythm, and desynchronization of stomach function.
. Studies show that hyperglycemia contributes to the slowing down of stomach emptying processes in both healthy and diabetic people. Hyperglycemia states are associated with reduced frequency of contractions of the stomach fundus, slowing of peristaltic action, development of abnormal rhythm, and desynchronization of stomach function.
Nervous system diseases![]() such as Parkinson's disease also pose a risk of gastroparesis. Thus, it is because neuropathy, or inflammation of the peripheral nerves, especially the vagus nerve, is closely related to gastroparesis. Parkinson's disease is a neurodegenerative ailment that causes damage to the nervous system. Neuropathies often occur in patients with Parkinson's disease.
such as Parkinson's disease also pose a risk of gastroparesis. Thus, it is because neuropathy, or inflammation of the peripheral nerves, especially the vagus nerve, is closely related to gastroparesis. Parkinson's disease is a neurodegenerative ailment that causes damage to the nervous system. Neuropathies often occur in patients with Parkinson's disease.
Paraneoplastic gastric motility disorders can occur in the course of cancer. In cancer patients, gastroparesis may be part of the paraneoplastic syndrome. Gastroparesis thus results from direct infiltration of the visceral plexus or vagus nerve, a history of surgery, chemotherapy, or radiation therapy. In addition to stomach and biliary tract cancer, small cell lung cancer![]() is also a risk for gastroparesis.
is also a risk for gastroparesis.

Amyloidosis is a rare group of conditions. Their common feature is the extracellular accumulation of insoluble protein in tissues and organs. Deposits of amyloid made up of abnormal light chains can damage peripheral nerves and the autonomic nervous system, causing neuropathy. Neuropathies![]() , on the other hand, can contribute to gastroparesis.
, on the other hand, can contribute to gastroparesis.
Intestinal ischemia is a set of symptoms that occur when there is a decrease in blood flow to the abdominal cavity caused by a blockage of one of the arteries supplying it. Atherosclerosis is the most common cause of chronic bowel ischemia. Intestinal ischemia is also mentioned as a cause of gastroparesis.
Postoperative gastroparesis can occur after procedures associated with the risk of vagus nerve damage, such as specific stomach procedures. It can occur after surgical treatment of obesity, as well as after duodenal resection. Damage to the vagus nerve results in loss of accommodation of the stomach and inhibition of its contractile function. On the other hand, Duodenal resection results in decreased plasma concentrations of motilin, which plays a role in emptying the stomach of food debris.
Some medications, such as opioids![]() or anticholinergic preparations, can contribute to gastroparesis. Known risk factors include the use of drugs that inhibit gastrointestinal peristalsis. Impaired gastrointestinal contractile function may worsen enteral feeding tolerance in these patients. Additional intestinal peristalsis is inhibited by poor eating habits, low physical activity, and stress.
or anticholinergic preparations, can contribute to gastroparesis. Known risk factors include the use of drugs that inhibit gastrointestinal peristalsis. Impaired gastrointestinal contractile function may worsen enteral feeding tolerance in these patients. Additional intestinal peristalsis is inhibited by poor eating habits, low physical activity, and stress.
Most often, however, gastroparesis is idiopathic. In many patients, no apparent cause for the condition can be determined. In some patients, the onset of idiopathic gastroparesis is preceded by a gastrointestinal or respiratory tract infection. In patients with post-infectious gastroparesis, the prognosis is better, the severity of symptoms is less, and there is often spontaneous improvement.
The symptoms of gastroparesis are mainly due to the backlog of food in the stomach. Symptoms are uncharacteristic and can confusingly point to various gastrointestinal diseases. In some cases, people with mild gastric motility disorders may not experience any symptoms, so the disease then runs its course without giving any signs, which makes diagnosis difficult.
Symptoms of gastroparesis include:

Symptoms of indigestion, that is, discomfort and pain in the epigastrium![]() , may occur. Epigastric pain is present most often in the idiopathic type of gastroparesis, where no clear cause is established. Abdominal pain is found in half of patients. In addition, epigastric pain is often the dominant symptom of gastroparesis.
, may occur. Epigastric pain is present most often in the idiopathic type of gastroparesis, where no clear cause is established. Abdominal pain is found in half of patients. In addition, epigastric pain is often the dominant symptom of gastroparesis.
Nausea-causing vomiting is also a common symptom of gastroparesis. Vomiting after some time can result in weight loss, malnutrition, or dehydration. It is then imperative to seek medical attention.
Bloating and feeling uncomfortable may occur. Flatulence is a feeling of uncomfortable fullness in the abdominal cavity, usually after a meal. In most cases, bloating is a subjective sensation unrelated to increased intestinal gas volume or abdominal girth resulting from a disruption of visceral sensation and intestinal motility.
Patients with gastroparesis may experience premature or excessive feeling of satiety. The feeling of an entire abdomen is unpleasant and associated with overeating, even though patients may not have eaten much. Gastroparesis is a condition that often results in weight loss![]() rather than weight gain.
rather than weight gain.
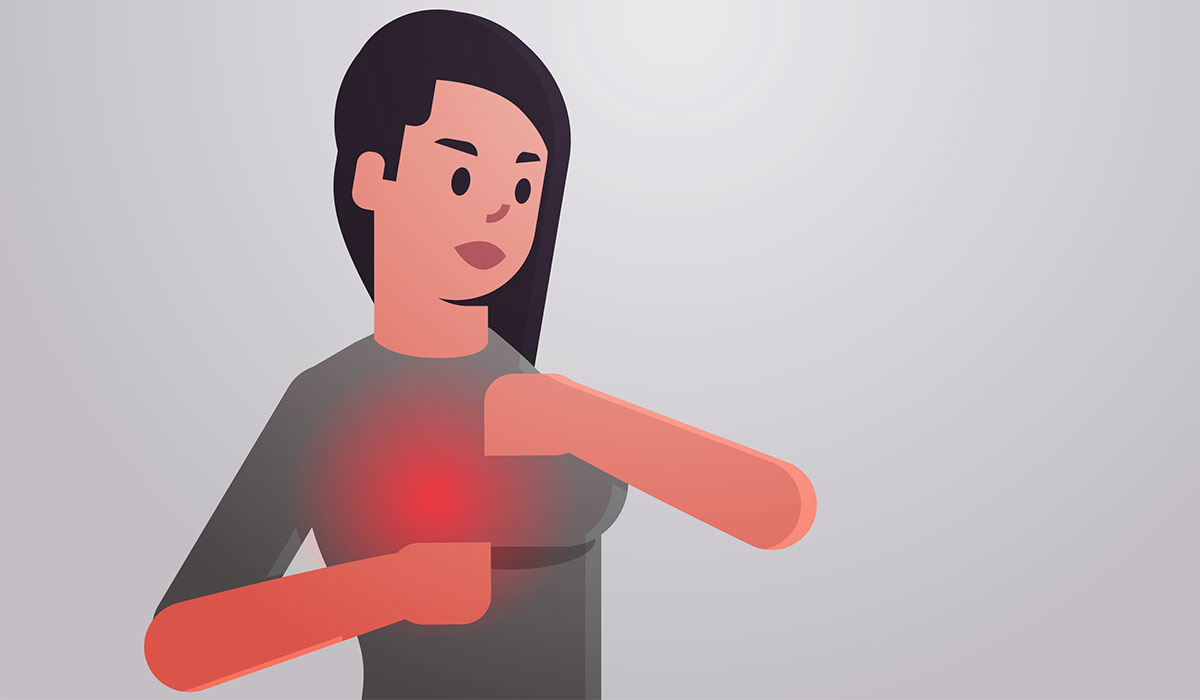
Due to food retention, heartburn and belching of food content can occur. Heartburn is an unpleasant ailment with a burning feeling in the chest and esophagus. It is associated with gastroesophageal reflux, the backflow of gastric juices into the esophagus.
Sometimes, hiccups are observed in patients with gastroparesis. Hiccups are a forced, synchronous contraction of the diaphragm and intercostal muscles. This contraction is triggered by a sudden inhalation followed by the closure of the glottis with a characteristic sound. It is a surviving, primitive reflex that protects the airway from aspiration of contents from the esophagus, i.e., choking.
Another rarer symptom of gastroparesis is dysphagia. Dysphagia is a term derived from Latin, meaning problems with swallowing. Dysphagia can affect both solid foods and liquids. Swallowing can be difficult or, in the most severe cases, impossible.

The symptoms of gastroparesis are so non-specific that the disease is difficult to diagnose. Similar symptoms are found in many different conditions. Gastroparesis is mainly differentiated from diseases such as peptic ulcer disease, reflux disease![]() , or thyroid gland dysfunction. A differential diagnosis is essential to rule out other conditions and provide appropriate treatment. Diagnostic methods for gastroparesis are based on an assessment of stomach emptying. Tests used in the diagnosis of gastroparesis include:
, or thyroid gland dysfunction. A differential diagnosis is essential to rule out other conditions and provide appropriate treatment. Diagnostic methods for gastroparesis are based on an assessment of stomach emptying. Tests used in the diagnosis of gastroparesis include:
The primary diagnostic method is scintigraphy after ingesting a special meal labeled with the radioactive isotope technetium. The method is also known as gastric emptying scintigraphy (GES). The test evaluates the level of gastric emptying several hours after eating a meal. Although many patients are noted to have normal or even accelerated gastric emptying, an optimally performed scintigraphic examination is practical and shows a good correlation with the presence of symptoms.
To rule out mechanical obstruction, an endoscopic examination of the upper gastrointestinal tract is performed. The assessment can be performed using the capsule method. The patient swallows a unique capsule equipped with a camera, and the examination is recorded in a particular receiving station. The endoscopic capsule, with the function of assessing pH, pressure, and temperature in the lumen of the gastrointestinal tract, makes it possible to measure the passage time through the various sections of the gastrointestinal tract, including the assessment of gastric emptying time.
A radiological examination with barium administration is also used in the diagnosis. In the examination, the shading agent barium sulfate is administered orally. This compound has the property of absorbing X-rays. The images obtained from such an examination represent the shape of the contracted gastrointestinal tract.
An alternative method of assessing stomach emptying is a breath test known as the gastric emptying breath test (GEBT)![]() . The test is done using a test meal containing a carbon isotope. The test takes samples of the air exhaled by the patient. The measure of gastric emptying rate is the isotope content of the exhaled air. The breath test is repetitive and comparable to the scintigraphy result. However, it may be unreliable in patients with malabsorption and respiratory diseases.
. The test is done using a test meal containing a carbon isotope. The test takes samples of the air exhaled by the patient. The measure of gastric emptying rate is the isotope content of the exhaled air. The breath test is repetitive and comparable to the scintigraphy result. However, it may be unreliable in patients with malabsorption and respiratory diseases.

The test is suitable for assessing stomach contractions. Manometry is good for identifying abnormalities in gastric and duodenal motility coordination. The test involves inserting a multichannel catheter through the nose into the stomach. However, the method can make patients uncomfortable. A few side effects may occur during esophageal manometry, such as watery eyes, discomfort in the nose and throat, nausea, and vomiting reflexes.
The examination allows assessment of the organs within the abdominal cavity. Ultrasound helps detect various conditions, which is why it is used in the differential diagnosis of gastroparesis. Abdominal ultrasound is, therefore, good for ruling out different causes of symptoms and confirming the correct disease entity in the patient.
Nutritional and pharmacological treatment is introduced if diagnostic tests confirm delayed stomach emptying without an existing mechanical obstruction. What is noteworthy is that treatment usually does not depend on the cause of the disease but on the patient's condition and the symptoms present. The exception is diabetic gastroparesis, in the treatment of which proper glycemic control is essential. The pharmacological treatment of gastroparesis is based on prokinetic medications, which accelerate gastric emptying.
Prokinetic drugs, which stimulate gastric motility, are used in treating gastroparesis. Short-term preparations of various substances can be used individually selected by the doctor. Prokinetic drugs are taken several minutes before meals. In addition, nausea-reducing and antiemetic drugs are included, if necessary.
In gastroparesis, nutritional treatment is essential. A proper diet can reduce malnutrition problems. It is recommended that meal portions be smaller but eaten more frequently. Eating fatty foods should be limited. Meals should be easily digestible. Alcohol consumption is not advisable. In a severe course of the disease, it may be necessary to take fragmented food.
In cases refractory to drug treatment or those with contraindications to medication, surgical treatment may be considered. Among the procedures performed are injection of the stomach pylorus with botulinum toxin and endoscopic or surgical pyloric plasty.

Untreated gastroparesis can cause complications that worsen the patient's condition. Very often, gastroparesis causes visible weight loss. However, in severe cases, it can even cause severe malnutrition![]() and related complications.
and related complications.
Upper gastrointestinal motility disorders are a common problem that causes progressive malnutrition. Malnutrition mainly manifests symptoms through decreased body weight and muscle and fat mass loss. Malnutrition is when insufficient amounts of certain nutrients, which are essential for proper functioning, are supplied to the body.
The condition is when the body's water content drops to a level that makes it difficult for the body to function correctly. A prolonged state of dehydration threatens our lives. The first signs of dehydration vary depending on whether the condition is mild or severe. In cases of mild dehydration, the patient complains of increased thirst, headaches, dizziness, and excessive weakness.
Malnutrition and dehydration can cause electrolyte disorders. Electrolytes are essential for the maintenance of homeostasis in a properly functioning body. A lack of electrolytes can lead to nervous system disorders and increased blood pressure. In more severe cases, in turn, it can result in fainting, convulsions, heart disorders, brittle bones, and paralysis.
Gastroparesis is a disorder that involves delayed or stopped emptying of the stomach due to damage to the nervous system responsible for controlling the function of this organ. Damage to the part of the nervous system responsible for maintaining the stomach contributes to delayed or stopped emptying of the stomach. It results in a backlog of food in the stomach, which results in unpleasant symptoms.
The etiology of the condition varies. Idiopathic gastroparesis is common, and in some patients, the condition is accompanied by diabetes. The symptoms of the disease are usually nausea and vomiting. The patient feels his abdomen is entire after a meal, and he usually feels satiety very quickly while eating. There may be bloating and feelings of discomfort.
The diagnosis of gastroparesis is possible only based on the co-occurrence of typical symptoms and the finding of delayed gastric emptying. The primary diagnostic method is scintigraphy after eating a meal labeled with a radioactive technetium isotope. In treating gastroparesis, most prokinetic drugs are used to stimulate gastric motility. Different treatments are also possible. It is essential to adjust the appropriate diet to promote gastroparesis.
Table of Contents
Gastritis is a common disease of the digestive system, characterized by various symptoms. See what causes this disease and learn… read more »

SIBO is a syndrome of symptoms that occurs when there are too many bacteria in the small intestine. The causes… read more »

H. pylori is a pathogenic bacterium. Untreated bacterial inflammation can lead to stomach cancer. Learn about treatment methods for Helicobacter… read more »
Stomach ulcer symptoms are easily recognizable. However, sometimes the disease is asymptomatic. See how to recognize stomach ulcer disease and… read more »
Heartburn is a common condition but it can also be a symptom of illness. Read the article and find out… read more »

GERD is a condition in which stomach contents flow back into the esophagus. If you feel heartburn and a burning… read more »
Zollinger-Ellison Syndrome is a condition that can cause uncharacteristic symptoms. Treatment is important as the disease can be fatal. Learn… read more »

A calorie is a determinant of the energy from the food consumed. Both calorie deficiency and excess cause harmful health… read more »
Mastitis is a condition that can affect many women, especially during the postpartum period. What symptoms does it cause? What… read more »