Ear Infections are various inflammatory conditions that require appropriate treatment. Accompanying inflammation is a serious problem that can occur in people of each age, regardless of gender. Inflammation of the ear can be mild and resolve spontaneously, but they can also pose a risk of complications, including hearing loss.
Ear infections can have various causes, depending on the type and location of the complaint—viruses and bacteria most often cause ear infections.
Ear infections occur when the external ear's defenses are damaged. Most of the symptoms of ear infections are non-specific and uncharacteristic. The most common symptoms of external ear infections are emerging pain and swelling. Ear infection treatment is selected on an individual basis, depending on the factor that is responsible for the development of the disease. The condition can affect the outer ear as well as the middle and inner ear. Ear infection should not be underestimated; if untreated, it can lead to dangerous complications, including meningitis.

An ear infection can have various causes and affect different ear parts. In addition, it can also vary in the intensity of the symptoms and the length of the illness. Various types of ear infections can, therefore, be distinguished.
The ear is an organ of hearing that consists of three parts. These include the outer ear, the middle ear, and the inner ear. The auricle and external auditory canal are part of the outer ear. A thin eardrum separates it from the middle ear. The middle ear, in turn, connects to the throat. The most hidden part of the ear is the inner ear, the most essential of which is the vagus. Ear infections can affect the outer, middle part, and inner parts. The following types of ear inflammation can, therefore, be listed:

External ear infection – Also called otitis externa. External ear infection affects the auricle and the external ear canal. This ailment is most common in children and adolescents. Factors favoring inflammation in the external ear include disruption of the epidermal barrier, decreased secretions, and a change in pH. The risk of external ear infections increases in people frequently using the swimming pool![]() .
.
Middle ear infection – Also called otitis media. Ear infection is a common childhood illness. In the first phase, this type of inflammation is a viral infection, but a bacterial infection may additionally occur during the disease. Ear infections are inflammations of the lining of the middle ear. You should know that otitis media can be associated with an upper respiratory illness.
Inner ear infection – Also called otitis interna or vaginitis. Inflammation of the inner ear can arise from long-term middle ear inflammation as a complication of inflammation within the auditory organ. Inflammation during this disease involves the vestibule, cochlea, and the three semicircular canals. With this type of ear infection, it is essential to implement treatment quickly, as the inflammatory process can spread, which is dangerous.
In addition, ear infections can also be divided into acute, exudative, and chronic. Chronic otitis media can result from untreated or inadequately treated acute otitis media in childhood. In contrast, exudative otitis media is an inflammation of the lining of the ear trumpet, the eardrum, and the air cells of the mastoid process. Exudative otitis media involves fluid accumulation in the eardrum cavity, which interferes with sound conduction and results in hearing impairment.

Many causes can lead to ear infections. Most commonly, it is infectious causes related to viruses and bacteria. But different causes are also possible and are worth considering for diagnosis. Determining the correct cause is critical to bringing in the proper treatment. The following causes of ear infections can, therefore, be distinguished:
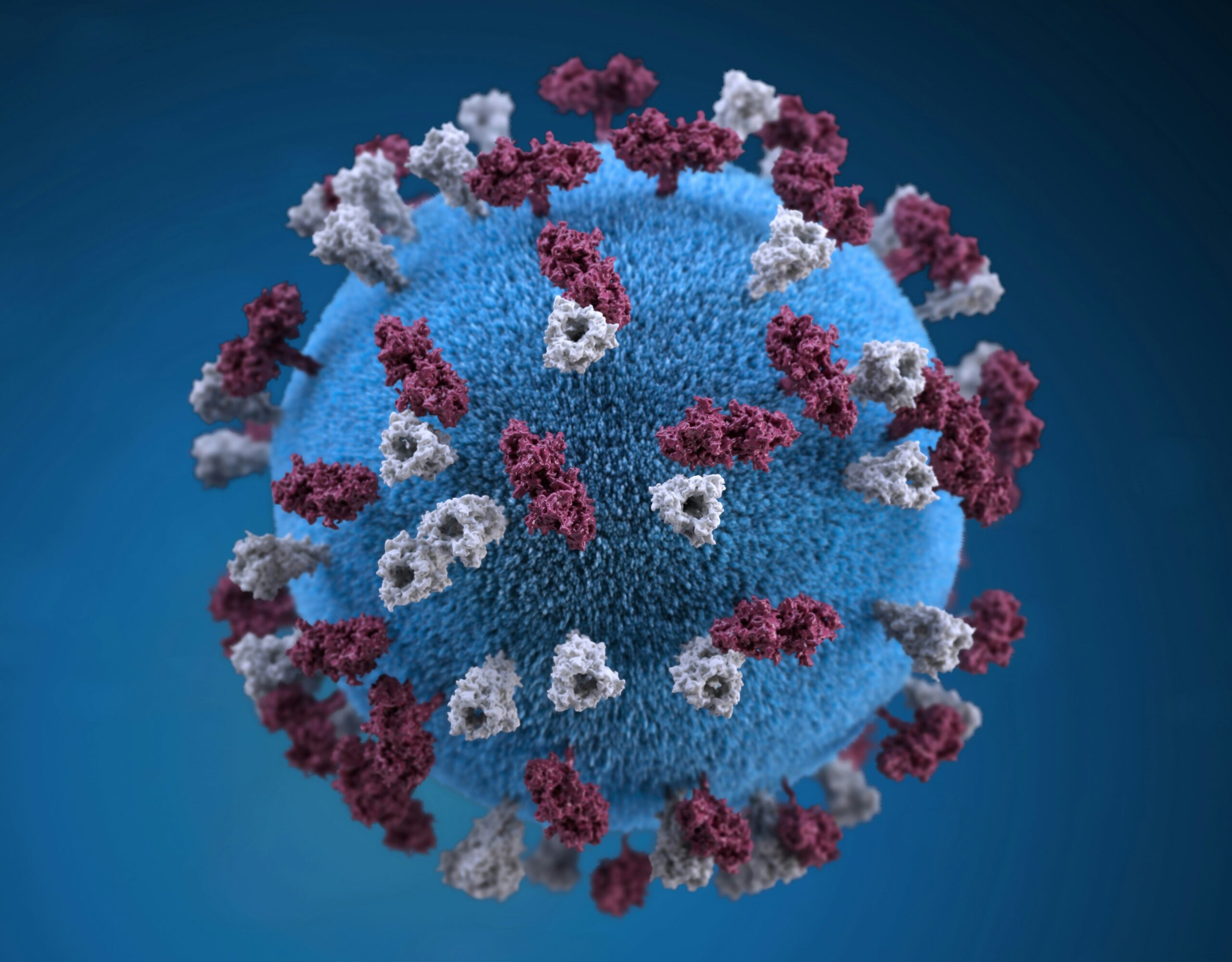
Viruses – Viruses can cause ear infections. Regarding otitis externa, the chickenpox virus![]() often plays a significant role in the disease. In addition, influenza viruses, rhinoviruses, adenoviruses, and RSV viruses are distinguished among the viruses responsible for ear problems. Inflammation can also occur if you have a viral or bacterial disease of the upper respiratory tract.
often plays a significant role in the disease. In addition, influenza viruses, rhinoviruses, adenoviruses, and RSV viruses are distinguished among the viruses responsible for ear problems. Inflammation can also occur if you have a viral or bacterial disease of the upper respiratory tract.
Bacteria – Bacterial infections most often cause ear infections. In cases of otitis externa, the most commonly isolated pathogens are Pseudomonas aeruginosa and Staphylococcus aureus. Streptococcus pneumoniae![]() , Haemophilus influenzae
, Haemophilus influenzae![]() and Moraxella catarrhalis
and Moraxella catarrhalis![]() cause acute otitis media. A multi-bacterial infection is also common. Thus, an ear infection like boils is also a bacterial infection.
cause acute otitis media. A multi-bacterial infection is also common. Thus, an ear infection like boils is also a bacterial infection.
Fungal infections – Other causes of ear infections include fungi. Fungi such as Aspergillus![]() or Candida
or Candida![]() are responsible for fungal ear infections. The microorganisms mentioned above physiologically colonize the nasal and oral cavities. However, when the human immune system is weakened, fungal populations overgrow and become health-threatening pathogens.
are responsible for fungal ear infections. The microorganisms mentioned above physiologically colonize the nasal and oral cavities. However, when the human immune system is weakened, fungal populations overgrow and become health-threatening pathogens.
Mechanical trauma – Damaged sebaceous glands, which cease to produce wax, may also be responsible for the development of external ear inflammation. Another possible cause of ear infections is the frequent use of ear sticks, leading to ear canal irritation. Changes in the pH of the ear canal are other possible causes of ear infections.
Allergies – Ear infections can also have an allergic origin. An allergic reaction can cause ear trumpet swelling, serous fluid retention in the ear, and, consequently, ear inflammation. Allergens are responsible for allergic ear infections. Various factors pose no threat to a healthy person, but in the case of allergy sufferers, the immune system perceives them as initiating a defense reaction.
Diseases – Various diseases can increase the risk of ear infections. This is especially true for systemic diseases, such as diabetes. Ear Infection can also occur following upper respiratory tract infections![]() , which include pharyngitis and laryngitis. In addition, the development of inflammation in this part of the ear can be favored by hypertrophy of the tonsil. Ear infections can also result from untreated inflammation in the middle ear, and autoimmune diseases can also cause it.
, which include pharyngitis and laryngitis. In addition, the development of inflammation in this part of the ear can be favored by hypertrophy of the tonsil. Ear infections can also result from untreated inflammation in the middle ear, and autoimmune diseases can also cause it.
Various symptoms accompany different types of infection. Ear Infection can occur suddenly in many patients. Ear infection symptoms in adults and children can produce very different symptoms, including what is related to, among other things, the cause that led to the inflammation and the place where the inflammation occurred. Ear infection symptoms include:

Pain – Most often, all ear infections are accompanied by pain in the ear![]() , which can be very intense and unpleasant. The pain is severe, unwelcome, and challenging to bear. In the case of otitis externa, the ear pain intensifies when chewing food or when pressure is applied to the auricle. In addition to it, there may also be a general headache and dizziness.
, which can be very intense and unpleasant. The pain is severe, unwelcome, and challenging to bear. In the case of otitis externa, the ear pain intensifies when chewing food or when pressure is applied to the auricle. In addition to it, there may also be a general headache and dizziness.
Swelling – A common symptom is swelling, congestion, and narrowing of the external ear canal. In the case of the middle ear, there is a protrusion of the eardrum. A swollen ear is also a manifestation of allergy. Swelling of the auricle may be a symptom of a contact allergy.
Itching – In some patients, the condition may manifest as annoying ear canal itching. Uncomfortable itching in the middle of the ear may indicate a fungal cause of the infection. Itching in the ears can also be associated with food allergies.
Ear effusion – Other symptoms include redness and an odorless or foul-smelling discharge![]() . The discharge can be noticed around the ears. The fluid oozes and dries on the skin. Initially, the exudate is watery, gradually changing to a thick discharge, causing a feeling of fullness and hearing loss. Depending on the cause of the discharge, pus, serous, or mucous fluid may leak from the ear.
. The discharge can be noticed around the ears. The fluid oozes and dries on the skin. Initially, the exudate is watery, gradually changing to a thick discharge, causing a feeling of fullness and hearing loss. Depending on the cause of the discharge, pus, serous, or mucous fluid may leak from the ear.
Blocked ear – A common symptom of ear infections is a feeling of a blocked ear, which reduces the listening experience. Additionally, it may be accompanied by pain or a sense of a foreign body in the ear. Pressure in the ear, resulting from a change in pressure, is also a common symptom. Pressure in the ear is a term that indicates a feeling of a filled ear.
Auditory symptoms – A blocked ear due to an infection can impair the hearing organ. Permanent hearing damage and even hearing loss can also result from ear infections. Tinnitus is also common in ear infections, squeaking feeling in the ear and a pulsating sensation.
Enlarged lymph nodes – Ear Infection of the external ear can result in enlarged lymph nodes that become painful to the touch. Enlarged lymph nodes behind the ear indicate an infection. Lymph nodes enlarge when a bacterial, viral, or fungal infection occurs. They can be felt with the fingers. In addition, it is often accompanied by fatigue and weakness.

The symptoms are mentioned when a bacterial or viral infection mainly causes flu-like symptoms that may accompany ear infections—for example, a fever![]() . The infection can also pass into the eardrum cavity from the nose or nasopharynx, causing flu-like symptoms.
. The infection can also pass into the eardrum cavity from the nose or nasopharynx, causing flu-like symptoms.
Recurrent upper respiratory tract infections, sinusitis, and palatal tonsil disease favor the development of chronic ear infections. Some patients may also present with different symptoms, which include nausea and vomiting. Additional complaints are observed depending on the form of chronic otitis media.
The diagnosis of Ear Infection requires a thorough history and physical examination due to the various causes and types of infection. Ear Infection treatment is selected individually, depending on the agent responsible for the development of the condition, so making the correct diagnosis is critical. Tests for ear infections include:

Otoscopic examination – Otoscopy![]() is fundamental in ear infections. It can reveal various degrees of inflammatory changes depending on the course of the disease. Otoscopy is another way of viewing the ear, done by an audiologist. The otoscope can visually assess the external ear canal and eardrum. It is possible to see a blurring of the light reflex, reddening and thickening of the entire eardrum, convexity, and reduced mobility.
is fundamental in ear infections. It can reveal various degrees of inflammatory changes depending on the course of the disease. Otoscopy is another way of viewing the ear, done by an audiologist. The otoscope can visually assess the external ear canal and eardrum. It is possible to see a blurring of the light reflex, reddening and thickening of the entire eardrum, convexity, and reduced mobility.
Pneumotoscopic examination – Pneumatic otoscopy![]() examination is a simple method of assessing eardrum mobility and diagnosing a range of middle ear conditions. The pneumatic otoscopy option and an attached pump for the examiner enable assessment of the mobility of an undamaged eardrum.
examination is a simple method of assessing eardrum mobility and diagnosing a range of middle ear conditions. The pneumatic otoscopy option and an attached pump for the examiner enable assessment of the mobility of an undamaged eardrum.
Audiological examination – Audiology examines pathologies within the sense of hearing. Audiology aims to detect the hearing impairment level, which is why it is carried out in an appropriately prepared, sound-attenuated booth. On the other hand, Tympanometry checks the condition of the middle ear, i.e., primarily the eardrum state and the ossicles' arrangement and rigidity. The fluid level in the tympanic cavity can also be verified during the examination.
CRP test – The CRP test is used in medical diagnosis to determine whether there is inflammation in the patient's body. A CRP test may indicate a developing bacterial ear infection if symptoms are present. An elevated test result is also a prognostic factor and allows for detecting complications following ear infections, such as an abscess.
Bacteriological examination – When a bacterial ear infection is suspected, bacteriological examination of ear, nose, and throat swabs is possible. This method allows for determining which pathogens have caused the inflammation and selecting appropriate antibiotics. Swabs are also possible for viral and fungal infections.

Depending on the cause of the disease, the method of treating the ear infection is tailored. In most patients, vigilant observation is recommended because the ear infections often are self-limiting![]() . It avoids unnecessary antibiotic therapy
. It avoids unnecessary antibiotic therapy![]() in the event of improvement. Symptomatic treatment is sufficient to alleviate the unpleasant symptoms of the ear infection. However, sometimes specialist treatment is needed. Treatments for ear infections include:
in the event of improvement. Symptomatic treatment is sufficient to alleviate the unpleasant symptoms of the ear infection. However, sometimes specialist treatment is needed. Treatments for ear infections include:

Antibiotic therapy – Treatment of ear Infections caused by bacteria involves the patient taking an antibiotic prescribed by their doctor. Antibiotics are available on the market in various types, but the most common are those in the form of ear drops. If additional symptoms occur with Ear Infection, which includes fever and headaches, it may be necessary to take appropriate oral antibiotics.
Antiviral treatment – Treatment is different if you are diagnosed with a viral ear infection. Antiviral drugs such as acyclovir may work well in the case of viral ear Infections. Antibiotics are ineffective for treating viral Ear Infections and are only used for bacterial infections.
Antifungal treatment – The patient should take antifungal medication if a fungal infection is the culprit of the ear infection. Treatment of fungal ear infections is based on clotrimazole and nystatin drops or powder. General antifungal preparations are recommended in cases of failure of topical therapy or immunosuppressed patients.
Pain treatment – Ear Infection is often associated with severe pain, significantly impairing the patient's functioning. For this goal, painkillers are administered to relieve the symptoms. Antipyretics may also be used for additional symptoms.
Anti-inflammatory treatment – Anti-inflammatory medication is also used to treat acute bacterial ear infections. Anti-inflammatory treatment is often used before antibiotic therapy is implemented. Anti-inflammatory drugs also work well where there are additional flu-like symptoms.
Mucolytic treatment – Mucolytic drugs dilute the secretions of the upper respiratory tract, making removing them from this area more accessible, and mucociliary transport is suitable for this goal. It thus helps to clear the airways of accumulated secretions. The treatment is helpful for ear infections accompanied by upper respiratory tract infections.
Nasal mucosal constricting drugs – Nasal mucosal constricting drugs to improve the permeability of the ear trumpet may work well for Ear Infections. Such drugs often contain the active ingredient xylometazoline hydrochloride, which has a vasoconstrictive effect and reduces swelling of the nasal mucosa.
Drainage of the tympanic cavity – Sometimes surgery is required to treat ear infections. In the case of long-term Ear Infection, a drainage of the eardrum cavity is done, which involves incising the eardrum and inserting a drain. It allows secretions to drain out and aerates the tympanic cavity. In most cases, leaving the drain in place for several months provides full recovery.
Incision of the tympanic membrane – Sometimes, incising the tympanic membrane or paracentesis is necessary. Indications for it are concurrent dizziness, nystagmus, facial nerve palsy, and insufficient spontaneous perforation of the tympanic membrane. In special situations, a procedure is done to close the defect in the eardrum and reconstruct the ossicular chain to improve hearing.
Untreated ear infections can lead to dangerous complications. These are most common in children, although they also occur in adults. They are divided into intranasal and intracranial—intra-temporal complications include vagus inflammation, facial nerve paresis, or paralysis. As for intracranial complications, these include meningitis![]() .
.
It is essential to focus on proper prevention to prevent the development of Ear Infections. Regular cleaning of the ear canal is recommended, among other things. You should also be careful when using a swimming pool and check that the water is not lingering in your ears. In addition, respiratory infections, a frequent complication of ear inflammation, should not be underestimated.
Ear Infections include different types of inflammation that need proper care. It's a serious issue that can hit anyone, regardless of age or gender. It has many triggers and can appear in different ear areas. Its symptoms and duration can also differ. Hence, we can classify different types of ear infections. There are numerous triggers for ear infections. Primarily, they relate to viruses and bacteria, but other factors are there, too, and should be considered during diagnosis. Identifying the right trigger helps bring the proper treatment into the picture.
Different infections come with other symptoms. Ear Infection can suddenly pop up in many people. Usually, an ear infection brings along with it ear pain, which can be severe and uncomfortable. Other signs include reddening and a discharge, which could be odorless or stinky. The treatment for the ear infection adjusts based on the cause. Careful observation is suggested in most patients with acute ear infections because symptoms often resolve themselves. This method helps avoid unnecessary antibiotic use if things get better.