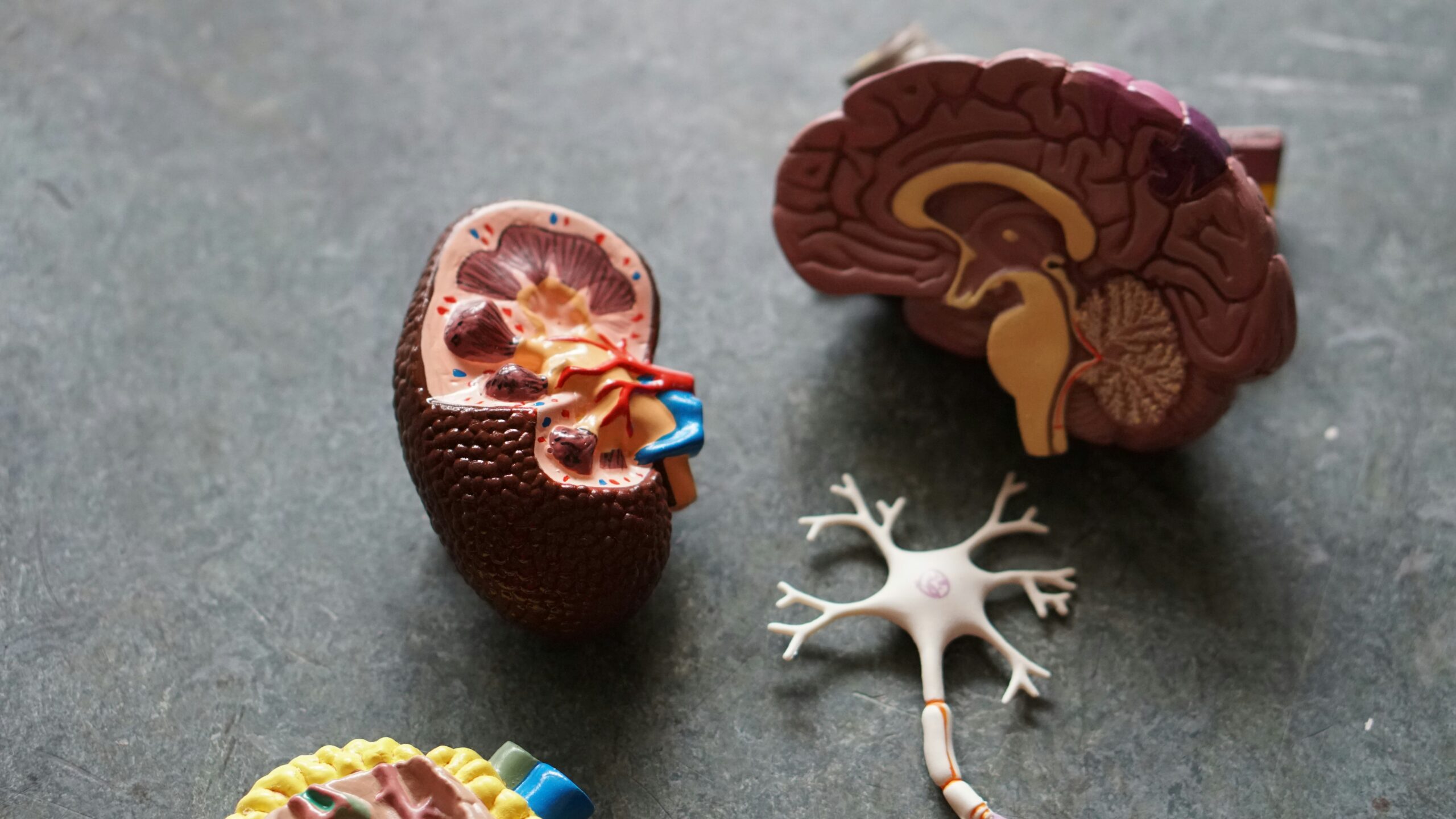
As a therapy, dialysis is nothing less than the brilliant discovery that enabled kidney failure patients to live longer. In renal replacement therapy, they have therapeutic uses. The kidneys are the primary blood-filtering organs in a human being. This fulfills the functions when these organs do not function through artificial equipment. As a result, dialysis can extract built-up metabolic substances and surplus fluid out of the blood. Doing so can give homeostasis to patients who are losing kidney function.
Kidney function loss is a major complication that stems from several diseases of these organs. A nephrologist determines the clinical condition and how patients qualify for dialysis. Dialysis ranges from short-term to lifelong kidney replacement therapy. Likewise, variable features characterize the different types of dialysis. The most common type is hemodialysis.
While the procedures demand proper patient preparation, dialysis therapy enables patients who have a severe chronic illness to sustain a good life quality for even decades. Nevertheless, remember that dialysis cannot be performed in many cases and that this intrusive technique can produce different complications in dialysis. Learn all about dialysis and life-saving therapy so you can be well-informed.

Through artificial machines that remove excess water, solutes, and toxins from the blood, dialysis can do work normally done by a kidney. The use of this kind of therapy is determined by the number of diseases that lead to kidney failure. 2010, for example, approximately 2.5 million![]() people worldwide were treated with this treatment.
people worldwide were treated with this treatment.
Many innovations and breakthroughs in medical technology have followed since pioneers such as Willem Kolff and Belding Scribner developed dialysis therapy, opening the way for many new possibilities so that patients can receive the help they need. With all these incredible therapies, we can break them down into three types. Dialysis can also be intermittent or continuous.
Hemodialysis removes blood from the body and cleans it through a specific system of bloodlines; this line leads to a machine that will purify your blood, known as the dialyzer. A dialyzer is a device for blood purification in which blood gets rid of toxins. In addition, with the help of dialysis fluid, electrolytes and acid-base balance are equalized. Re-infusions cleaned blood from harmful metabolic waste products and excessive fluids into the patient.
Most hemodialysis patients are treated in specialized hospital units. The key to obtaining this treatment is obtaining good and effective access to the patient's circulation through an arteriovenous fistula, catheter, or prosthesis. The patient must also be able to endure fluctuations in blood pressure and blood levels of poisonous metabolic byproducts.

Peritoneal dialysis is a meta-dialysis that uses the intrinsic filtering ability of the membrane lining the abdominal cavity from within. This very membrane has tiny pores that are used as an outlet for harmful metabolic products to be eliminated from the body. In PD dialysis, the peritoneal cavity is filled with dialysis fluid. A catheter is inserted, and the fluid passes through the catheter into the peritoneal cavity, where it purifies blood. Those patients who prefer this technique appreciate the autonomy and independence peritoneal dialysis provides.
It can be done at home and also has better mobility for patients. Although currently a minority of the dialysis population in the USA, peritoneal dialysis Those who need dialysis have to choose between hemodialysis and peritoneal dialysis. The decision should be directed towards the patient based on counseled deliberation over all relevant factors impacting treatment effectiveness.
In case of severe kidney damage, a special therapy is necessary—renal replacement therapies. Of these, continuous renal replacement therapy (CRRT) is growing in favor of intermittent hemodialysis and prolonged intermittent renal replacement therapy. CRRT encompasses continuous techniques for solute depletion and net fluid handling.
This necessitates patients being attached to a machine that performs kidney function 24/7. For hemodynamically unstable patients, the intervention is ideal for controlled fluid management and minimizes the risk of disease complications. Through a semi-permeable membrane, CRRT filters blood through passive diffusion and ultrafiltration.
The frequency and duration of each dialysis treatment and the specific composition of the concentrate used in the filtration process are individualized based on patient state. We provide examples of how to recognize indications for different types of dialysis. Doctors call the shots on whether a patient is dialyzed — and tell patients it must be done. Pathological conditions in which dysregulation and impairment of immune response modulators occur, leading to wide varieties of harm, are indications for dialysis. These are vasodilation, cardiac depression, and immunosuppression, causing end-organ injury, hemodynamic instability, or slow renal recovery.

Acute kidney injury happens when the kidneys suddenly stop functioning. Infections, cancer, medications, and autoimmune diseases are a few of the conditions that can damage our kidneys. These patients need treatment until the kidneys function normally once again. Not all treatment requires dialysis; some cases only require antibiotic therapy. However, the medication varies immensely for what is causing it and how sick the individual is. Factors that determine the timing to initiate dialysis in acute kidney injury are refractory patients or uremia-symptom-related disorders.
Neurological complications of chronic kidney disease on conservative treatment are a clear indication for renal replacement therapy. Uremic encephalopathy is due to slow metabolism of brain tissue and impaired release of neurotransmitters. It is a clinical disorder in which symptoms associated with untreated uremia occur. It only occurs sporadically now due to access to dialysis and the timely start of renal replacement therapy. A clinical syndrome characterized by increasingly quantitative and qualitative disturbances of consciousness, which represents the symptoms of encephalopathy. Id mainly lethargy, fatigue, decreased attention, and headache. Over time, patients may also develop tremors before uremic coma.
In certain cases of severe renal failure, it produces uremic pericarditis. It is due to the detrimental effects of urea and toxins that have built up in the blood, leading to pericardial cell injury, oxidative stress, and, subsequently, inflammation. The main symptom of chest pain in acute pericarditis is chest pain behind the sternum or surrounding the heart. Treatment depends on the reason or cause and its seriousness. May need dialysis for uremic pericarditis.
Dialysis is possible for the patient, though life-threatening hyperkalemia may be a pyrrole. Hyperkalemia — too many potassium parts in the blood. Abnormal potassium levels can impact the functioning of the nervous system, muscles, and heart. It is also the most important hyperkalemia disorder in the water and electrolyte balance of the body. If potassium is in excess, it will be excreted by the kidneys with urine and can cause weakness in the organs. The main cause of this situation is the administration of medications that inhibit renal potassium excretion in patients with chronic kidney disease.

Hypervolemia is another scenario that may warrant dialysis. It refers to excessive water retention in the body. In patients with kidney failure, the cause of excess water in the body may be an excessive fluid supply. Individuals suffering from heart failure, nephrotic syndrome, or cirrhosis may also develop conductivity. Edema is the prime feature of water retention in the body. Patients who have developed organ complications, for example, lung edema due to conductance, need to be treated with dialysis.
Acidosis is a dangerous situation characterized by the disturbed acid-base balance in which acids have the upper hand. The lungs and kidneys also help maintain normal pH values. Severe metabolic acidosis, particularly if kidney damage has occurred, can require dialysis. Immediate treatment is required, as metabolic acidosis can be a life-threatening condition.
Chronic kidney disease patients develop complications like protein and calorie malnutrition. Regular nutritional care is important when treating this disease. Early treatment can also prevent nutritional deficits. Dialysis might be needed in severely malnourished patients.
It is now also recognized that hemodialysis may be effective and appropriate in many forms of toxicologic poisoning. These substances can be drugs, methanol, and fungi. Based in these toxins can harm the kidneys and bring about kidney failure. Excessive alcohol can also affect these organs and cause them to need dialysis.
Absolute or relative contraindications to different forms of dialysis exist and are context-specific. Local anesthesia, along with careful nursing coercion, can overcome psychological contraindications, including dislike of needles. However, there are situations where a patient has made clear they do not want dialysis, and the provider must uphold that wish.
If vascular access cannot be provided, hemodialysis has an absolute contraindication. Dialysis requires inserting a catheter in the patient or forming a fistula. This is done through vascular access, where blood drawn from the patient's circulatory system gets purified in the dialyzer and later returned to his body. Achieving dialysis efficacy and improving quality of life rely on adequate vascular access and exquisite care. There are three types of vascular access currently used in hemodialysis. An arteriovenous fistula is the primary and preferred permanent vascular access method. Dialysis may also not be possible due to difficult vascular access.
Dialysis is associated with cardiovascular complications when continued over a long duration. There are even fatal cases. Following dialysis, the heart gets less blood and oxygen. And this is when the trouble starts, as the heart needs to pump more. Ultimately, the heart can become so distended it cannot pump any blood effectively, which results in heart failure and death. For those with existing heart failure, though, dialysis is a risk-filled no-go zone.
The medical term coagulopathy is an enveloping word for the condition of a blood clotting disorder. Blood clotting is important to stop bleeding from the damaged vessel and prevent hemorrhage. For the same reason, even for dialysis, a mere fistula/catheter is risky in such patients. Dialysis outcomes can also be affected by dialysis-associated complications like severe coagulopathy that complicates extracorporeal blood purification.
The following conditions should be met if peritoneal dialysis is used. Patients with uncorrected abdominal wall hernia or abdominal adhesions may be able to dialyze, but such patients cannot undergo peritoneal dialysis. This also complicates the pleuroperitoneal fistula. Multiple abdominal surgeries leading to dense scarring and adhesions or fistulas are, therefore, contraindications to peritoneal dialysis.
Likewise, CRRT has some contraindications. CRRT may be insufficient if patient outcomes are needed more quickly than this intervention can provide. The following conditions may less favorably influence the use of this type of dialysis, as patients are recommended for dialysis by clinicians; lack of centers with sufficient expertise or organ supportive equipment makes practice variable; and permanent liver failure in ineligible for liver transplantation![]() patients.
patients.

Young dialysis patients have markedly higher mortality rates than age-matched control subjects, primarily due to complications. Effective interprofessional collaboration is required to avert the worst possible outcome for hemodialysis patients. Finally, we describe potential complications related to various types of uremic dialysis.
A complication of dialysis is intradialysis hypotension, including the higher prevalence of regional wall motion abnormalities during dialysis, referred to as myocardial stunning. Nonetheless, mortality tracks quite closely with below-normal systolic blood pressure. More commonly seen as vertigo, photophobia followed by nausea. Symptoms can be insidious and require great medical attention. Ultrafiltration should be reduced rapidly, and vital signs should be carefully monitored until the level of functionality is stable. HD patients have a relatively twofold increased risk![]() for cardiac arrest than PD patients three months after commencing dialysis.
for cardiac arrest than PD patients three months after commencing dialysis.
Certain reactions are medical emergencies and require immediate cessation of dialysis, tightening of the line, and supportive management followed by definitive care. Cases like this one are known as dialysis imbalance syndrome. The neurological disorder is manifested by a neurological deficit that can sometimes result in a coma. It results from the influx of water into the CNS due to dialysis. If you add an osmotic agent to the blood, this will be avoided.
This complication can occur at any time immediately after dialysis because of a response to the ethylene oxide used to sterilize dialyzers. Intravenous drug administration is part of the treatment. Nonspecific dialyzer reactions may lead to a range of symptoms.
While dialysis is a vital treatment for addressing electrolyte imbalances, it can induce such an imbalance. Electrolyte disturbances are common in hemodialysis and CRRT, potentially affecting several electrolytes. Hypocalcemia![]() , hypokalemia
, hypokalemia![]() , and hypophosphatemia
, and hypophosphatemia![]() are the most frequent electrolyte abnormalities that occur during hemodialysis. This group of patients, many who have electrolyte abnormalities, are especially vulnerable to these on CRRT. Intravenous or oral supplementation will treat electrolyte deficiencies.
are the most frequent electrolyte abnormalities that occur during hemodialysis. This group of patients, many who have electrolyte abnormalities, are especially vulnerable to these on CRRT. Intravenous or oral supplementation will treat electrolyte deficiencies.
Peritoneal dialysis has a risk of infections. Infection of the abdominal cavity is the most serious complication, and if the risk of dialysis increases due to this failure, it can be a threat to life. Abdominal pain and turbid peritoneal fluid are the main features of most infections. Local examinations should also be carried out now and then on dialysis patients to look for signs of infection.