Blood clots are your body's way of stopping you from bleeding too much. Blood has an ostensibly unimaginable assignment: it must flow constantly and smoothly throughout your organism for an entire lifetime but shut off quickly to avoid spills when you get an injury or wound.
A type of blood cell called platelets teams up with plasma, the liquid part of your blood, to stop bleeding by creating a clot over any injury you have. Once you heal the injury, your body should break down the blood clot.
Blood clots are beneficial and lifesaving when they prevent you from bleeding out. However, they may also develop when they are not required and lead to a heart attack, stroke, or other severe medical problems.
Correct, undisturbed blood flow![]() in blood vessels is one of the guarantees of the proper functioning of the body. The balance between clotting and clot dissolution (fibrinolysis
in blood vessels is one of the guarantees of the proper functioning of the body. The balance between clotting and clot dissolution (fibrinolysis![]() ) is maintained by a precise system called the hemostasis system.
) is maintained by a precise system called the hemostasis system.
The hemostasis system consists of:
All these components ensure uninterrupted, undisturbed blood flow – hemostasis![]() . Coagulation is a process in which many proteins and messengers participate. A damaged blood vessel triggers a cascade of reactions that involve:
. Coagulation is a process in which many proteins and messengers participate. A damaged blood vessel triggers a cascade of reactions that involve:
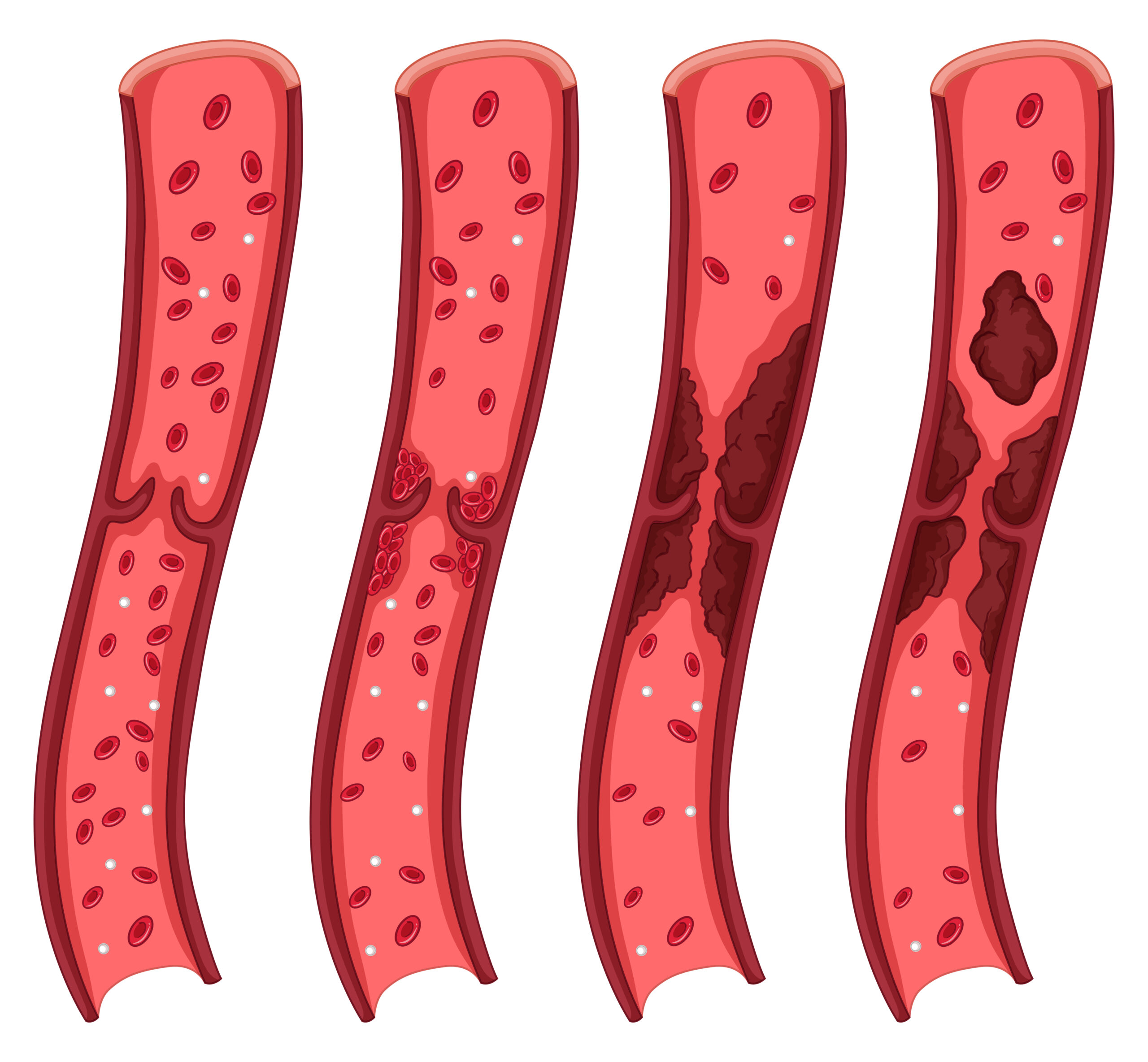
Activation of the coagulation system![]() is like dominoes falling over each other. The beginning cascade reaction of activation of the next factor by the previous one transforms the last soluble fibrinogen into insoluble fibrin, creating a clot. At the same time, platelets adhere to each other and the site of vessel damage, forming a platelet plug that prevents blood from flowing out. The fibrinolysis process occurs after successfully stopping the bleeding, dissolving the blood clot
is like dominoes falling over each other. The beginning cascade reaction of activation of the next factor by the previous one transforms the last soluble fibrinogen into insoluble fibrin, creating a clot. At the same time, platelets adhere to each other and the site of vessel damage, forming a platelet plug that prevents blood from flowing out. The fibrinolysis process occurs after successfully stopping the bleeding, dissolving the blood clot![]() . Clot-dissolving enzymes are activated, ensuring the patency of the vessel.
. Clot-dissolving enzymes are activated, ensuring the patency of the vessel.
In a healthy circulatory system, blood flows rapidly through the veins to the heart. The working muscles facilitate the blood movement from the legs in the direction opposite to the force of gravity. The valves in the veins stop blood from rushing downwards. If the blood wants to turn back, they snap shut and block the way back.
If any of the elements of this mechanism fails, blood pools in the veins, which leads to inflammation and then damage to the epithelial layer lining the vessel – the endothelium.
At injury sites, platelets “stick” to the endothelium and each other, forming a thrombus. It reduces the diameter of blood vessels, thus hindering the outflow of peripheral blood to the heart.
The body's reaction to a blood clot varies. Sometimes, it is absorbed – but then the valves and internal walls of the vein within it are damaged, and the formation of new clots is only a matter of time. Sometimes, they form a clot during absorption – however, it may happen after many months or years.
If the body does not absorb the clot, it can grow so large that it blocks the vein like a cork. Although it usually plugs the deep veins of the lower leg, this situation favors the formation of new clots and their spread to the popliteal and femoral veins. They will surround subsequent valves and prevent them from working typically.
Blood clot problems are associated with numerous diverse conditions types. A blood clot can develop because the patient cuts, and their organism works to stop the bleeding. Some disorders, such as bleeding disorders or blood clotting issues, concentrate on blood clots. The individual can also suffer from diseases that increase the risk of developing blood clots.
Having a bleeding disorder![]() means the patient's blood does not clot as it should, and the individual is at risk of bleeding uncontrollably if they get injured. Bleeding disorders include:
means the patient's blood does not clot as it should, and the individual is at risk of bleeding uncontrollably if they get injured. Bleeding disorders include:
A blood clotting disorder![]() (hypercoagulable state) is a situation that causes the organism to produce more blood clots than standard. Individuals may inherit conditions that raise the chance of blood clots or develop those conditions during their lifetime. Standard blood clotting diseases include:
(hypercoagulable state) is a situation that causes the organism to produce more blood clots than standard. Individuals may inherit conditions that raise the chance of blood clots or develop those conditions during their lifetime. Standard blood clotting diseases include:
Many risk factors![]() can increase blood clot risk. They include:
can increase blood clot risk. They include:
Mostly, blood clots are not dangerous![]() and dissolve on their own. However, in some cases, they may lead to harmful and potentially life-threatening medical conditions.
and dissolve on their own. However, in some cases, they may lead to harmful and potentially life-threatening medical conditions.
Deep venous thrombosis![]() is the formation of blood clots, usually in the veins of the legs.
is the formation of blood clots, usually in the veins of the legs.
Most often, it begins in the veins in the calf muscles, and from there, passing into larger and larger veins, it can travel upwards to the veins in the thigh and sometimes even in the pelvis and abdominal cavity. In rare cases, fragments of clots may break off and travel with the bloodstream toward the heart and lungs, causing pulmonary embolism. It is often asymptomatic, which the patient learns about during other tests.
If the clot is large enough, when it reaches the lungs, it may cause obstruction, i.e., embolism of the pulmonary artery or its branches.
If the clogged vessel has a large diameter, its closure causes infarction and death of a large part of the lung, which may cause severe disease symptoms, such as:
Sometimes, the clot breaks away from the vessel wall and flows with the blood through the heart to the pulmonary artery![]() . If the clots are small, they partially block the vessel. A large clot causes pulmonary embolism, which may result in acute circulatory failure and sudden death.
. If the clots are small, they partially block the vessel. A large clot causes pulmonary embolism, which may result in acute circulatory failure and sudden death.
Pulmonary artery blockage may be indicated by stabbing chest pain, shortness of breath, fever, cough (sometimes coughing up blood), balance disorders, and loss of consciousness. Any disorders in the respiratory system require quick intervention by a specialist.
Unfortunately, embolism is often preceded by no symptoms. In such cases, the doctor may have problems stating the diagnosis and starting appropriate treatment.
The prevention![]() of developing dangerous blood clots depends on the degree of risk of the disease.
of developing dangerous blood clots depends on the degree of risk of the disease.
Thrombosis![]() is one of the most common related to blood clot complications of surgical procedures and internal diseases. Specialists have conducted studies in many countries, concluding that thrombosis prevention is still insufficient. It is necessary to systematically educate doctors and inform patients and their families so that knowledge of thrombosis risk factors is common – which may be the most effective method of preventing thrombotic complications.
is one of the most common related to blood clot complications of surgical procedures and internal diseases. Specialists have conducted studies in many countries, concluding that thrombosis prevention is still insufficient. It is necessary to systematically educate doctors and inform patients and their families so that knowledge of thrombosis risk factors is common – which may be the most effective method of preventing thrombotic complications.
The most significant risk concerns bedridden people with limited mobility and patients who have undergone major surgeries, especially orthopedic ones. However, these people are often under medical care and receive subcutaneous injections of the so-called low molecular weight or unfractionated heparin. The duration of such prevention depends on the length of the patient's immobilization and the type of disease he suffers from.
A separate issue is the indications and type of antithrombotic prophylaxis that should be used in healthy people who stay home and demonstrate standard physical activity. These people have life situations and medical conditions in which the risk of thrombosis may also be increased.
Currently, three methods of preventing thrombosis are known, used separately or in combination.
An anticoagulant drug![]() is administered to the patient to treat existing clots or as a part of prevention – in situations with an increased risk of their formation (e.g., after surgery).
is administered to the patient to treat existing clots or as a part of prevention – in situations with an increased risk of their formation (e.g., after surgery).
Sometimes, they are also used to preserve blood samples taken for testing. The most popular preparations are heparin, a chemical compound inhibiting thrombin formation.
Anticoagulants should always be used as directed by your doctor. Not only is their appropriate dosage significant, but so is the form they take. Anticoagulants are available mainly in the form of tablets or injections.
The term compression therapy![]() mainly covers the use of compression garments and intermittent pneumatic compression treatment.
mainly covers the use of compression garments and intermittent pneumatic compression treatment.
Compression garments![]() (stockings and knee-high socks) are designed to pressure the superficial veins in the legs, allowing blood to flow faster back to the heart. This prevents blood from pooling and prevents clots from forming. Compression garments with dosed pressure can be used for most people. It is worn mainly by people in hospitals undergoing surgery. Stockings and knee-high socks can be used both alone and in combination with drug treatment.
(stockings and knee-high socks) are designed to pressure the superficial veins in the legs, allowing blood to flow faster back to the heart. This prevents blood from pooling and prevents clots from forming. Compression garments with dosed pressure can be used for most people. It is worn mainly by people in hospitals undergoing surgery. Stockings and knee-high socks can be used both alone and in combination with drug treatment.
Intermittent pneumatic compression![]() is a treatment that concerns inflatable sleeves that fit around the legs. The sleeve is attached to a machine that periodically inflates the sleeves with air to create pressure around the limbs and then deflates them. As in the case of compression garments, its advantage is that the procedure can be performed on most patients, including pregnant women.
is a treatment that concerns inflatable sleeves that fit around the legs. The sleeve is attached to a machine that periodically inflates the sleeves with air to create pressure around the limbs and then deflates them. As in the case of compression garments, its advantage is that the procedure can be performed on most patients, including pregnant women.
Thrombosis may damage venous valves, which leads to obstructed blood flow from the legs towards the heart and accumulation in the ankle joints. Exercises that activate the calf muscles affect the so-called muscle pump. Muscles tighten and relax to help blood flow to the heart.
Recommended exercises![]() for preventing blood clot forming include:
for preventing blood clot forming include:

In a normal pregnancy, a woman without additional risk factors should remember to exercise regularly, tighten her calf muscles, and flex her feet. It is advisable to rest with your legs raised, and if you experience swelling in your calves, wear preventive compression knee socks and sleep with your legs slightly higher.
Pregnant women![]() who have had venous thrombosis in the past should be sure to inform their doctor about this fact, as additional prevention with heparin may be necessary. You should also inform your doctor about thrombosis and pulmonary embolism cases in close family members. It is also worth discussing these issues with your doctor when planning your pregnancy.
who have had venous thrombosis in the past should be sure to inform their doctor about this fact, as additional prevention with heparin may be necessary. You should also inform your doctor about thrombosis and pulmonary embolism cases in close family members. It is also worth discussing these issues with your doctor when planning your pregnancy.
To avoid the so-called economy class syndrome![]() , healthy people usually need to hydrate their bodies well before traveling, wear loose clothing, and do calf exercises, such as flexing the feet and tensing the calf muscles during the trip.
, healthy people usually need to hydrate their bodies well before traveling, wear loose clothing, and do calf exercises, such as flexing the feet and tensing the calf muscles during the trip.
When traveling by car or bus, breaks in the journey and brisk walking are recommended, as they tense the calf muscles, stimulating venous outflow from the calves.
People with risk factors for thrombosis (e.g., they have already had a thrombosis, are obese, have large varicose veins, or suffer from chronic diseases) should agree on the method of prevention with their doctor before the planned treatment because, in their case, it may be advisable to administer a one-time preventive injection of heparin.
To sum up, here are recommended activities to do to prevent developing thrombosis: